I’ve previously written about ultrarunning preparation and a little bit about how I approach fueling. But it occurred to me there might be others out there wondering exactly HOW to find fuel that works for them, because it’s an iterative process.
The way I approach fueling is based on a couple of variables.
First and foremost, everything has to be gluten free (because I have celiac). So that limits a lot of the common ultrarunning fuel options. Things like bars (some are GF, most are not), Uncrustables, PopTarts, and many other common recommendations in the ultra community just aren’t an option for me. Some, I can find or make alternatives to, but it’s worth noting that being gluten free for celiac (where cross-contamination is also an issue, not just the ingredients) or having a food allergy and being an ultrarunner can make things more challenging.
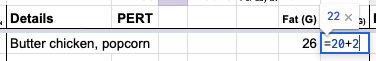
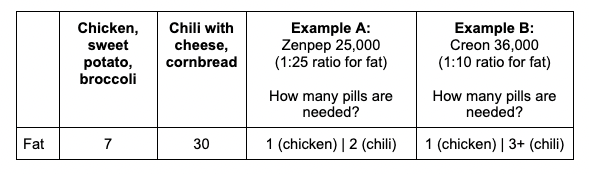
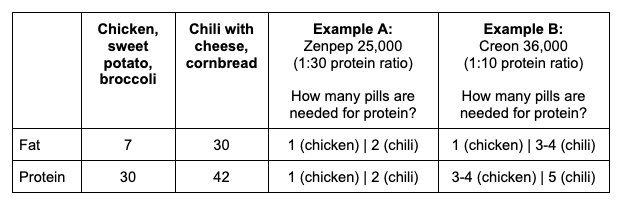
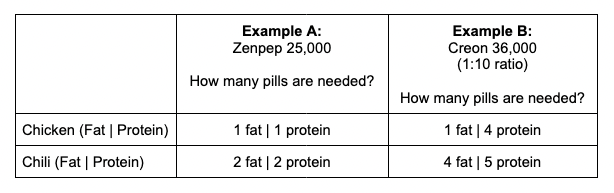
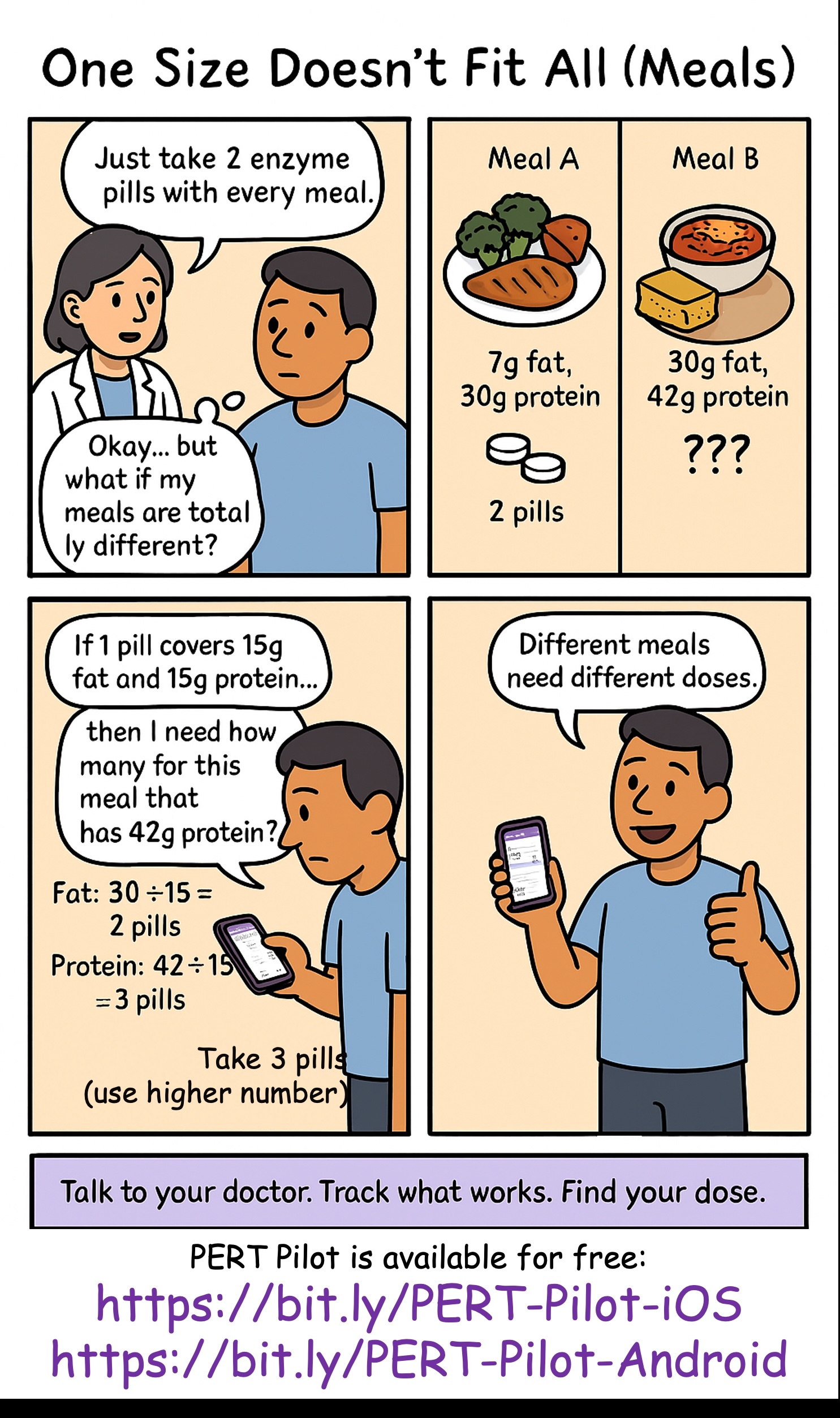
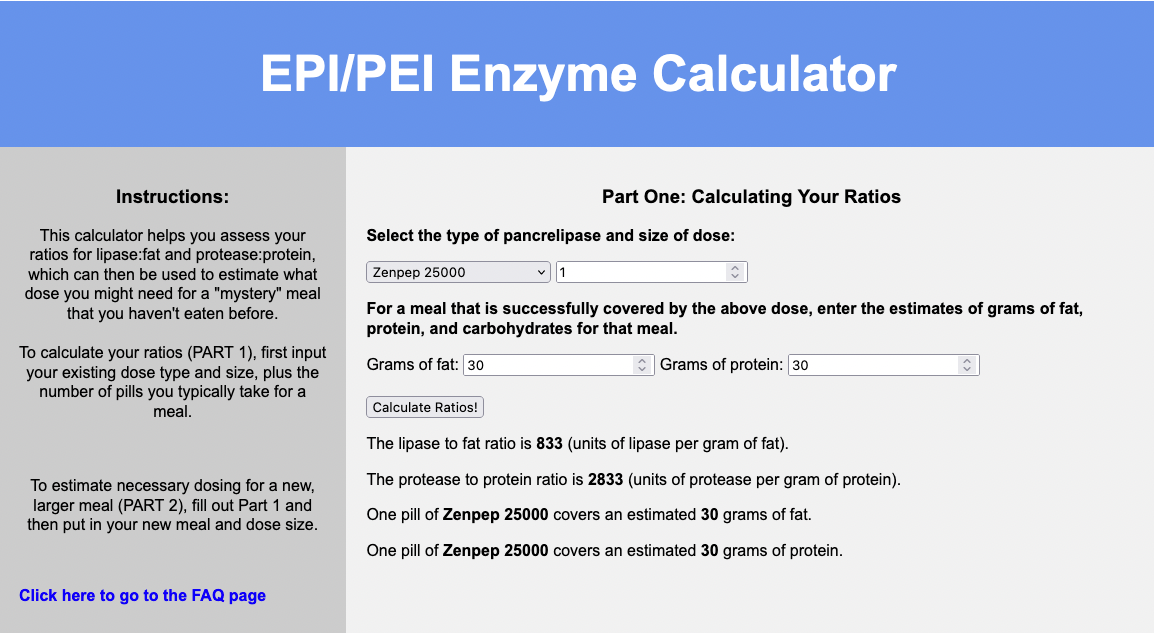
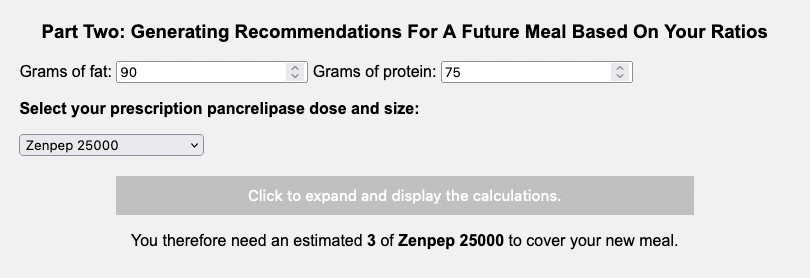
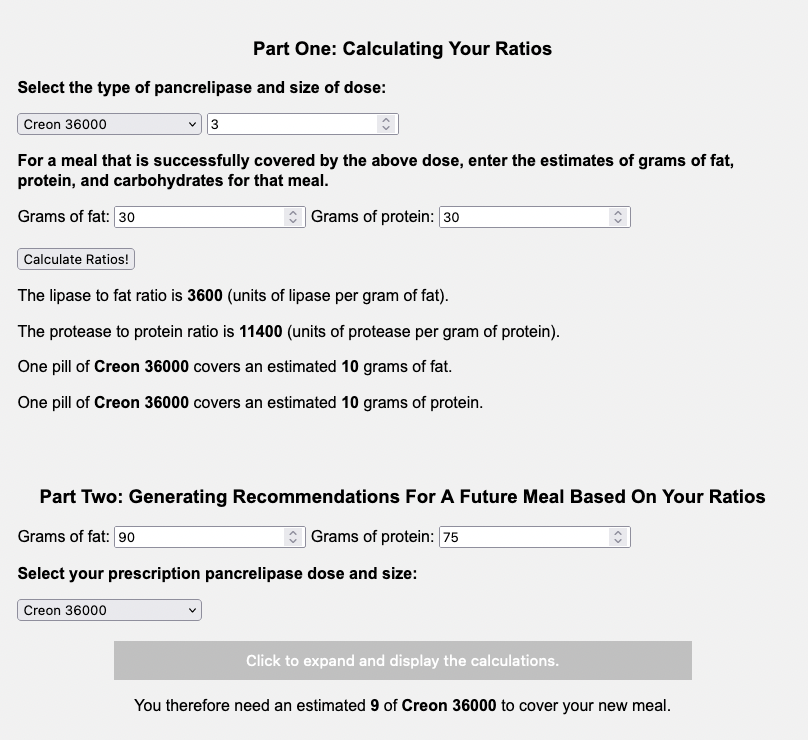
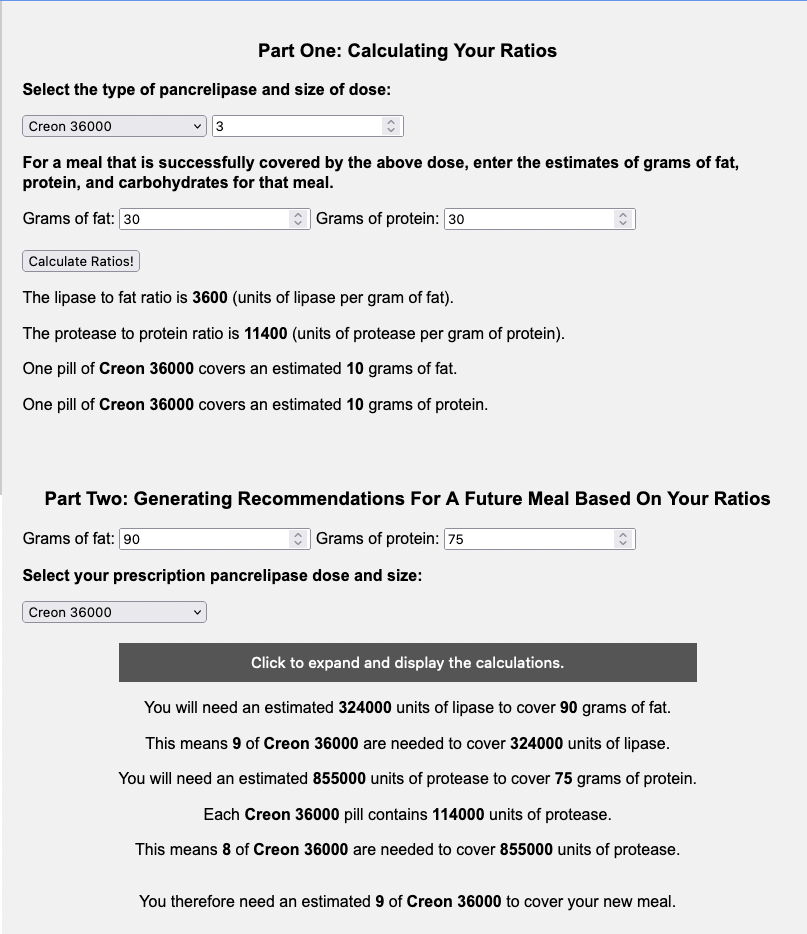
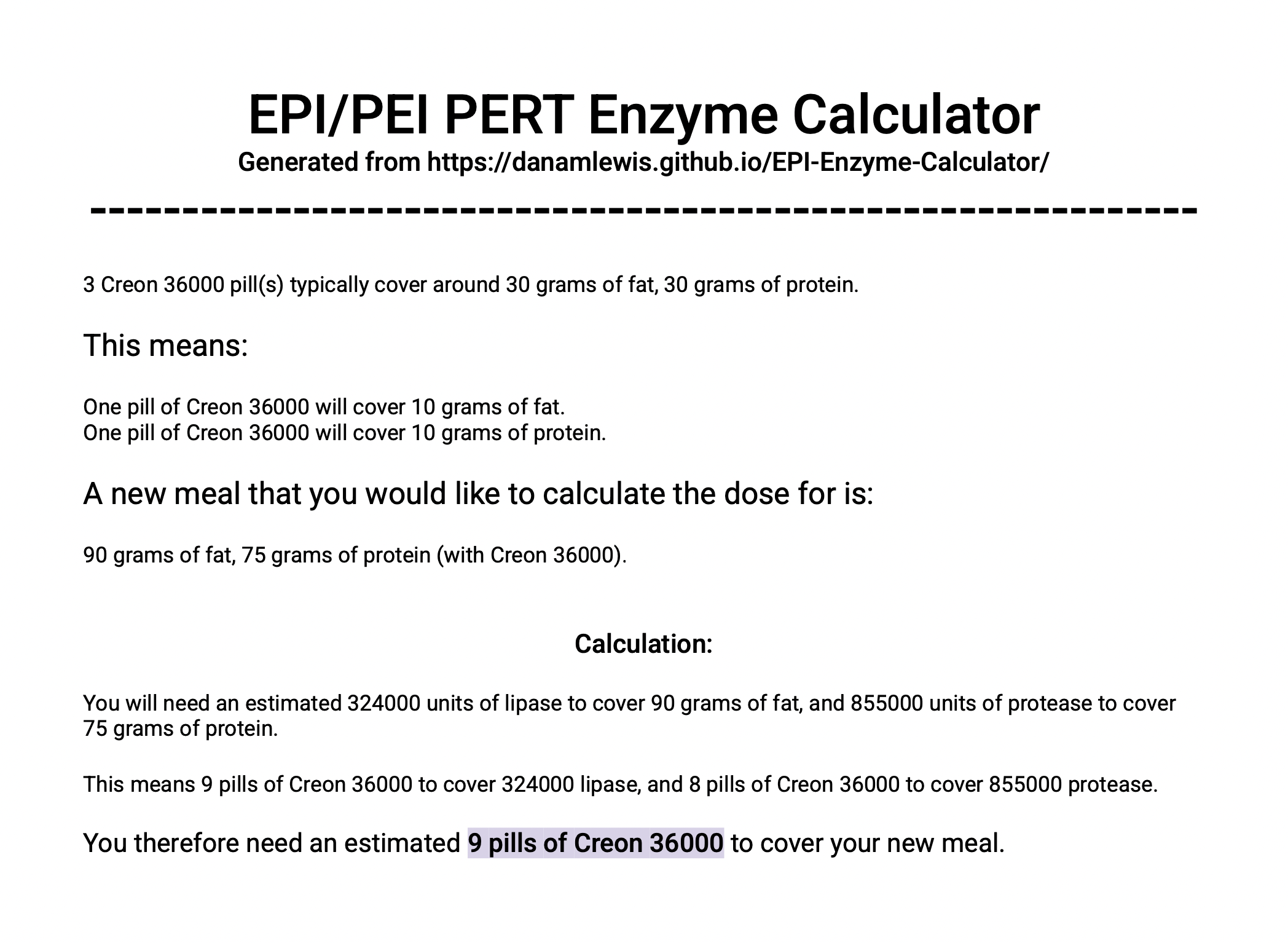
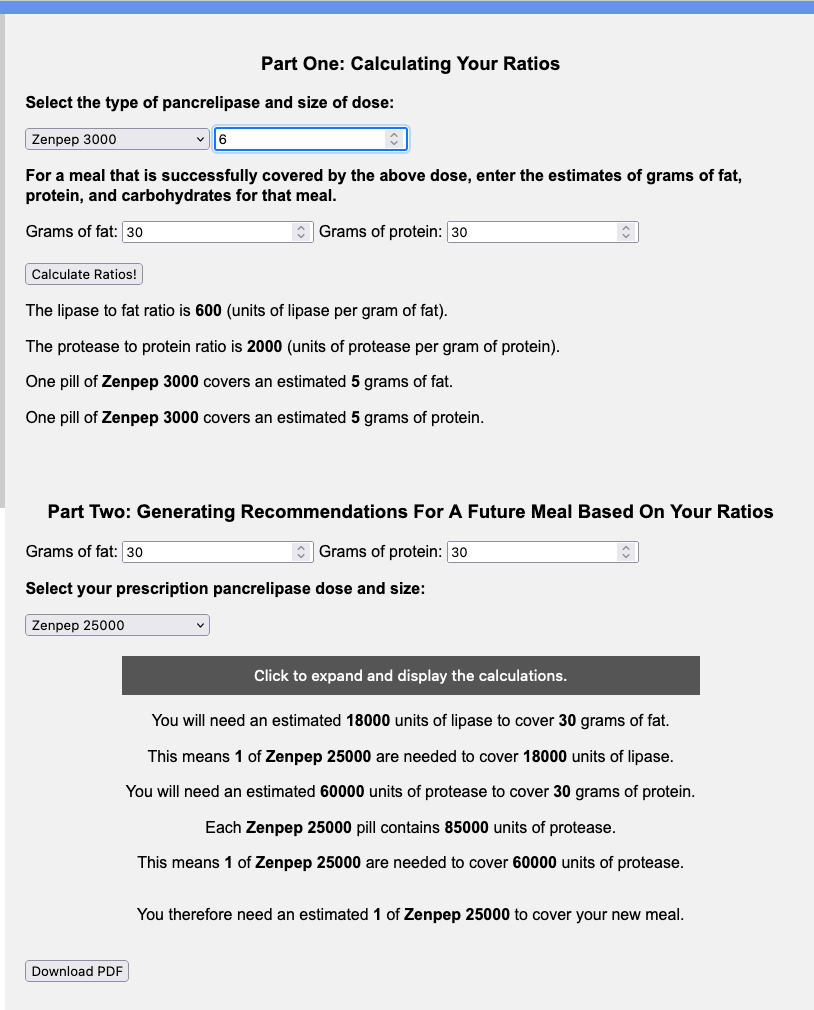
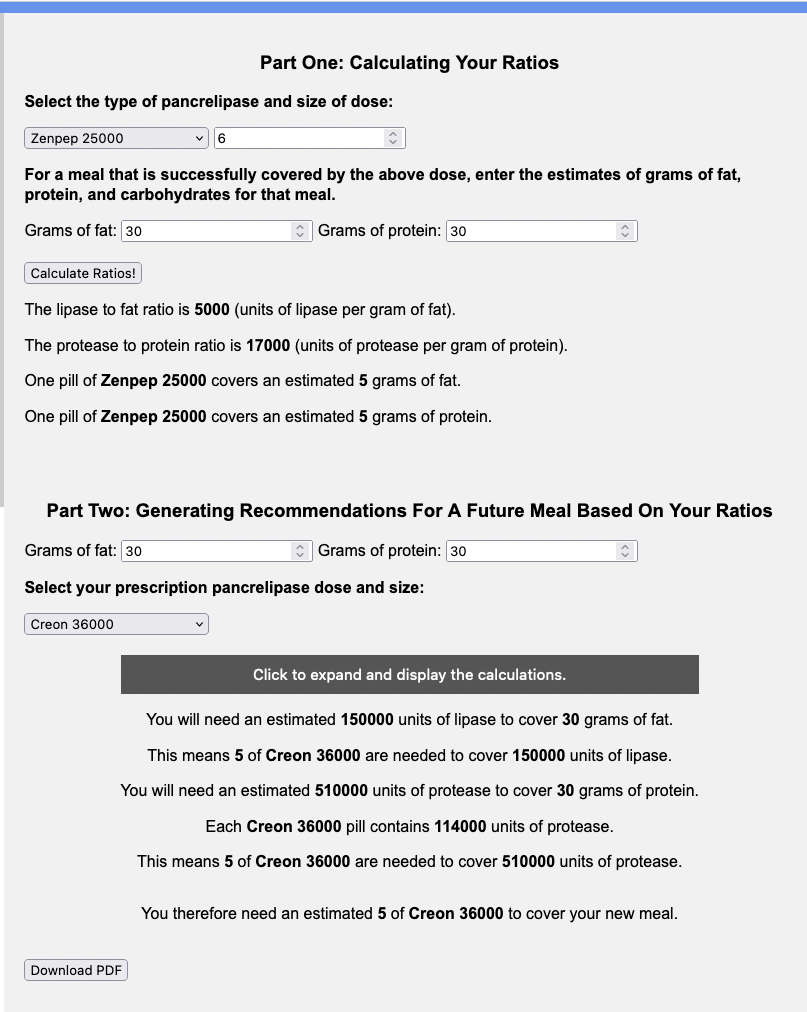
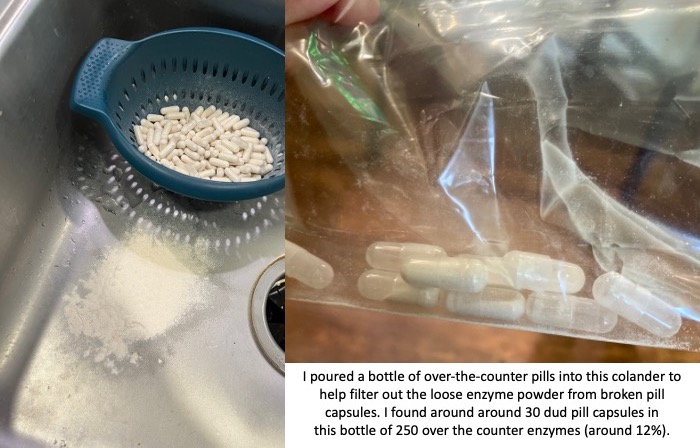
Then, I also have exocrine pancreatic insufficiency. This doesn’t limit what I eat, but it factors in to how I approach ideal fueling options, because I have to match the enzyme amounts to the amount of food I’m eating. So naturally, the pill size options I have of OTC enzymes (one is lipase only and covers ~6g of fat for me, the other is a multi-enzyme option that includes protease to cover protein, and only enough lipase to cover ~4g of fat for me; I also have one much larger that covers ~15g of fat but I don’t typically use this one while running) influence the portion sizes of what I choose.
That being said, I probably – despite EPI – still tend toward higher fat options than most people. This is in part because I have had type 1 diabetes for 20+ years. While I by no means consume a low c-a-r-b diet, I typically consume less than the people with insulin-producing pancreases in my life, and lean slightly toward higher fat options because a) my taste buds like them and b) they’ve historically had less impact on my glucose levels. Reason A is probably the main reason now, thanks to automated insulin delivery, but regardless of reason, 20+ years of a higher level than most people’s fat consumption means I’m also probably better fat-adapted for exercise than most people.
Plus, ultrarunning tends to be slower than shorter runs (like marathons and shorter for most people), so that’s also more amenable to fat and other nutrient digestion. So, ultrarunners in general tend to have more options in terms of not just needing “gu” and “gel” and “blocks” and calorie-sugar drinks as fuel options (although if that is what you prefer and works well for you, great!).
All of these reasons lead me toward generally preferring fuel portions that are:
- Gluten free with no cross-contamination risk
- ~20g of carbs
- ~10g of fat or less
- ~5-10g of protein or less
Overall, I shoot for consuming ~250 calories per hour. Some people like to measure hourly fuel consumption by calories. Others prefer carb consumption. But given that I have a higher tolerance for fat and protein consumption – thanks to the enzymes I need for EPI plus decades of practice – calories as a metric for hourly consumption makes sense for me. If I went for the level of carb intake many recommend for ultrarunners, I’d find it harder to consistently manage glucose levels while running for a zillion hours. I by no means think any of my above numbers are necessarily what’s best for anyone else, but that’s what I use based on my experiences to date as a rough outline of what to shoot for.
After I’ve thought through my requirements: gluten free, 250 calories per hour, and preferably no single serving portion size that is greater than 20ish grams of carbs or 10g of fat or 5-10g or protein, I can move on to making a list of foods I like and that I think would “work” for ultrarunning.
“Work” by my definition is not too messy to carry or eat (won’t melt easily, won’t require holding in my hands to eat and get them messy).
My initial list has included (everything here gluten free):
- Oreos or similar sandwich type cookies
- Yogurt/chocolate covered pretzels
- PB or other filled pretzel nuggets
- Chili cheese Fritos
- Beef sticks
- PB M&M’s
- Reese’s Pieces
- Snickers
- Mini PayDays
- Macaroons
- Muffins
- Fruit snacks
- Fruit/date bars
- GF (only specific flavors are GF which is why I’m noting this) of Honey Stinger Stroopwaffles
I wish I could include more chip/savory options on my lists, and that’s something I’ve been working on. Fritos are easy enough to eat from a snack size baggie without having to touch them with my hands or pull individual chips out to eat; I can just pour portions into my mouth. Most other chips, though, are too big and too ‘sharp’ feeling for my mouth to eat this way, so chili cheese Fritos are my primary savory option, other than beef sticks (that are surprisingly moist and easy to swallow on the run!).
Some of the foods I’ve tried from the above list and have eventually taken OFF my list include:
- PB pretzel nuggets, because they get stale in baggies pretty fast and then they feel dry and obnoxious to chew and swallow.
- Muffins – I tried both banana muffin halves and chocolate chip muffin halves. While they’re moist and delicious straight out of the oven, I found they are challenging to swallow while running (probably because they’re more dry).
- Gluten free Oreos – actual Oreo brand GF Oreos, which I got burnt out on about the time I realized I had EPI, but also they too have a pretty dry mouthfeel. I’ve tried other brand chocolate sandwich cookies and also for some reason find them challenging to swallow. I did try a vanilla sandwich cookie (Glutino brand) recently and that is working better – the cookie is harder but doesn’t taste as dry – so that’s tentatively on my list as a replacement.
Other than “do I like this food” and “does it work for carrying on runs”, I then move on to “optimizing” my intake in terms of macronutrients. Ideally, each portion size and item has SOME fat, protein, and carbs, but not TOO MUCH fat, protein and carbs.
Most of my snacks are some fat, a little more carb, and a tiny bit of protein. The outlier is my beef sticks, which are the highest protein option out of my shelf-stable running fuel options (7g of fat, 8g of protein). Most of the others are typically 1-3g of protein, 5-10g of fat (perfect, because that is 1-2 enzyme OTC pills), and 10-20g of carb (ideal, because it’s a manageable amount for glucose levels at any one time).
Sometimes, I add things to my list based on the above criteria (gluten free with no cross-contamination list; I like to eat it; not messy to carry) and work out a possible serving size. For example, the other day I was brainstorming more fuel options and it occurred to me that I like brownies and a piece of brownie in a baggie would probably be moist and nice tasting and would be fine in a baggie. I planned to make a batch of brownies and calculated how I would cut them to get consistent portion sizes (so I would know the macronutrients for enzymes).
However, once I made my brownies, and started to cut them, I immediately went “nope” and scratched them off my list for using on runs. Mainly because, I hate cutting them and they crumbled. The idea of having to perfect how to cook them to be able to cut them without them crumbling just seems like too much work. So I scratched them off my list, and am just enjoying eating the brownies as brownies at home, not during runs!
—
I first started taking these snacks on runs and testing each one, making sure that they tasted good and also worked well for me (digestion-wise) during exercise, not just when I was sitting around. All of them, other than the ones listed above for ‘dry’ reasons or things like brownies (crossed off because of the hassle to prepare), have stayed on the list.
I also started looking at the total amount of calories I was consuming during training runs, to see how close I was to my goal of ~250 calories per hour. It’s not an exact number and a hard and fast “must have”, but given that I’m a slower runner (who run/walks, so I have lower calorie burn than most ultrarunners), I typically burn in the ballpark of ~300-400 calories per hour. I generally assume ~350 calories for a reasonable average. (Note, again, this is much lower than most people’s burn, but it’s roughly my burn rate and I’m trying to show the process itself of how I make decisions about fuel).
Aiming for ~250 calories per hour means that I only have a deficit of 100 calories per hour. Over the course of a ~100 mile race that might take 30 hours, this means I’ll “only” have an estimated deficit of 3,000 calories. Which is a lot less than most people’s estimated deficit, both because I have a lower burn rate (I’m slower) and because, as described above and below, I am trying to be very strategic about fueling for a number of reasons, including not ending up under fueling for energy purposes. For shorter runs, like a 6 hour run, that means I only end up ~600 calories in deficit – which is relatively easy to make up with consumption before and after the run, to make sure that I’m staying on top of my energy needs.
It turns out, some of my preferred snacks are a lot lower and higher calories than each other! And this can add up.
For example, fruit snacks – super easy to chew (or swallow without much chewing). 20g of carb, 0g of fat or protein, and only 80 calories. Another easy to quickly chew and swallow option: a mini date (fruit) bar. 13g carb, 5g fat, 2 protein. And…90 calories. My beef stick? 7g of fat, 8g of protein, and only 100 calories!
My approach that works for me has been to eat every 30 minutes, which means twice per hour. Those are three of my favorite (because they’re easy to consume) fuel options. If I eat two of those in the same hour, say fruit snacks and the date bar, that’s only 170 calories. Well below the goal of 250 for the hour! Combining either with my beef stick (so 180 or 190 calories, depending), is still well below goal.
This is why I have my macronutrient fuel library with carbs, fat, protein, *and* calories (and sodium, more on that below) filled out, so I can keep an eye on patterns of what I tend to prefer by default – which is often more of these smaller, fewer calorie options as I get tired at the end of the runs, when it’s even more important to make sure I’m at (or near) my calorie goals.
Tracking this for each training run has been really helpful, so I can see my default tendency to choose “smaller” and “easier to swallow” – but that also means likely fewer calories – options. This is also teaching me that I need to pair larger calorie options with them or follow on with a larger calorie option. For example, I have certain items on my list like Snickers. I get the “share size” bars that are actually 2 individual bars, and open them up and put one in each baggie. ½ of the share size package (aka 1 bar) is 220 calories! That’s a lot (relative to other options), so if I eat a <100 calorie option like fruit snacks or a date bar, I try to make it in the same hour as the above average option, like the ½ snickers. 220+80 is 300 calories, which means it’s above goal for the hour.
And that works well for me. Sometimes I do have hours where I am slightly below goal – say 240 calories. That’s fine! It’s not precise. But 250 calories per hour as a goal seems to work well as a general baseline, and I know that if I have several hours of at or greater than 250 calories, one smaller hour (200-250) is not a big deal. But this tracking and reviewing my data during the run via my tracking spreadsheet helps make sure I don’t get on a slippery slope to not consuming enough fuel to match the demands I’m putting on my body.
And the same goes for sodium. I have read a lot of literature on sodium consumption and/or supplementation in ultrarunning. Most of the science suggests it may not matter in terms of sodium concentration in the blood and/or muscle cramps, which is why a lot of people choose sodium supplementation. But for me, I have a very clear, distinct feeling when I get not enough sodium. It is almost like a chemical feeling in my chest, and is a cousin (but distinct) feeling to feeling ketones. I’ve had it happen before on long hikes where I drank tons to stay hydrated and kept my glucose levels in range but didn’t eat snacks with sodium nor supplement my water. I’ve also had it happen on runs. So for me, I do typically need sodium supplementation because that chemical-like feeling builds up and starts to make me feel like I’m wheezing in my chest (although my lungs are fine and have no issues during this). And what I found works for me is targeting around 500mg/hour of sodium consumption, through a combination of electrolyte pills and food.
(Side note, most ultrarunning blogs I’ve read suggest you’ll be just fine based on food you graze at the aid station. Well, I do most of my ultras as solo endeavors – no grazing, everything is pre-planned – and even if I did do an organized race, because of celiac I can’t eat 95% of the food (due to ingredients, lack of labeling, and/or cross contamination)…so that just doesn’t work for me to rely on aid station food to supplement me sodium-wise. But maybe it would work for other people, it just doesn’t for me given the celiac situation.)
I used to just target 500mg/hour of sodium through electrolyte pills. However, as I switched to actually fueling my runs and tracking carbs, fat, protein, and calories (as described above), I realized it’d be just as easy to track sodium intake in the food, and maybe that would enable me to have a different strategy on electrolyte pill consumption – and it did!
I went back to my spreadsheet and re-added information for sodium to all of my food items in my fuel library, and added it to the template that I duplicate for every run. Some of my food items, just like they can be outliers on calories or protein or fat or carbs, are also outliers on sodium. Biggest example? My beef stick, the protein outlier, is also a sodium outlier: 370mg of sodium! Yay! Same for my chili cheese Fritos – 210mg of sodium – which is actually the same amount of sodium that’s in the type of electrolyte pills I’m currently using.
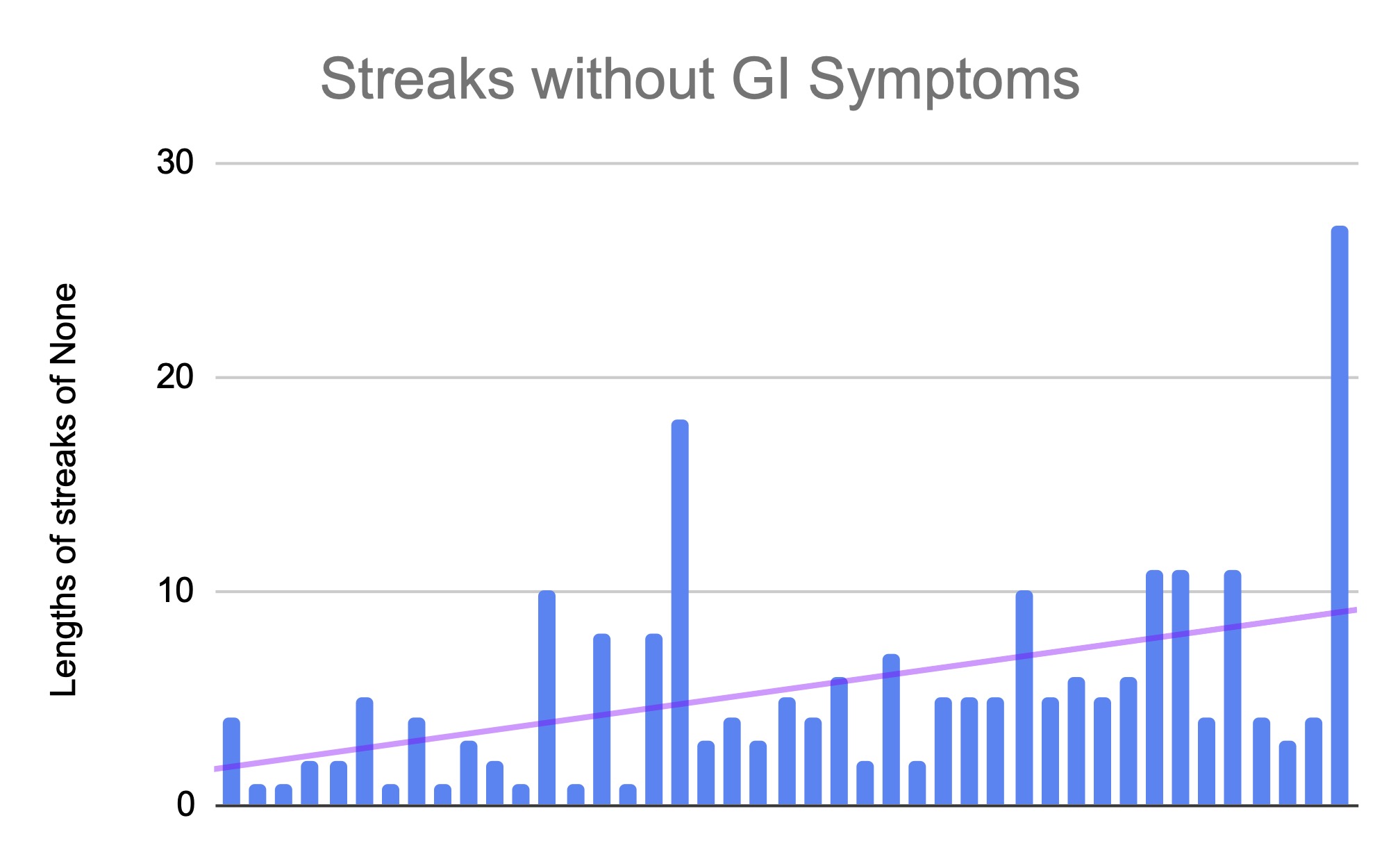
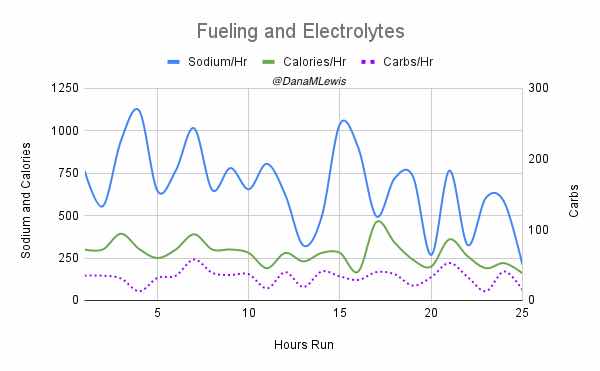
I originally had a timer set and every 45 minutes, I’d take an electrolyte pill. However, in the last year I gradually realized that sometimes that made me over by quite a bit on certain hours and in some cases, I ended up WAY under my 500mg sodium goal. I actually noticed this in the latter portion of my 82 mile run – I started to feel the low-sodium chest feeling that I get, glanced at my sheet (that I hadn’t been paying close attention to because of So. Much. Rain) and realized – oops – that I had an hour of 323mg of sodium followed by a 495mg hour. I took another electrolyte pill to catch up and chose some higher sodium snacks for my next few fuels. There were a couple hours earlier in the run (hours 4 and 7) where I had happened to – based on some of my fresh fuel options like mashed potatoes – to end up with over 1000mg of sodium. I probably didn’t need that much, and so in subsequent hours I learned I could skip the electrolyte pill when I had had mashed potatoes in the last hour. Eventually, after my 82-mile run when I started training long runs again, I realized that keeping an eye on my rolling sodium tallies and tracking it like I tracked calories, taking an electrolyte pill when my hourly average dropped <500mg and not based on a pre-set time when it was >500mg, began to work well for me.
And that’s what I’ve been experimenting with for my last half dozen runs, which has worked – all of those runs have ended up with a total average slightly above 500mg of sodium and slightly above 250 calories for all hours of the run!
Now, you may be wondering – she tracks calories and sodium, what about fat and protein and carbs?
I don’t actually care about or use these in real-time for an hourly average; I use these solely as real-time decision in points as 1) for carbs, to know how much insulin I might need dependent on my glucose levels at the time (because I have Type 1 diabetes); and 2) the fat and protein is to make sure I take the right amount of enzymes so I can actually digest the fuel (because I have exocrine pancreatic insufficiency and can’t digest fuel without enzyme pills). I do occasionally look back at these numbers cumulatively, but for the most part, they’re solely there for real-time decision making at the moment I decide what to eat. Which is 95% of the time based on my taste buds after I’ve decided whether I need to factor in a higher calorie or sodium option!
For me, my higher sodium options are chili cheese Fritos, beef stick, yogurt covered pretzels.
For me, my higher calorie options are the ½ share size Snickers; chili cheese Fritos; Reese’s pieces; yogurt covered pretzels; GF honey stinger stroopwaffle; and 2 mini PayDay bars.
Those are all shelf-stable options that I keep in snack size baggies and ready to throw into my running vest.
Most of my ‘fresh’ food options, that I’d have my husband bring out to the ‘aid station’/turnaround point of my runs for refueling, tend to be higher calorie options. This includes ¼ of a GF PB&J sandwich (which I keep frozen so it lasts longer in my vest without getting squishy); ¼ of a GF ham and cheese quesadilla; a mashed potato cup prepared in the microwave and stuck in another baggie (a jillion, I mean, 690mg of sodium if you consume the whole thing but it’s occasionally hard to eat allll those mashed potatoes out of a baggie in one go when you’re not actually very hungry); sweet potato tots; etc.
So again, my recommendation is to find foods you like in general and then figure out your guiding principles. For example:
- Do you have any dietary restrictions, food allergies or intolerances, or have already learned foods that your body Does Not Like while running?
- Are you aiming to do carbs/hr, calories/hr, or something else? What amounts are those?
- Do you need to track your fuel consumption to help you figure out how you’re not hitting your fuel goals? If so, how? Is it by wrappers? Do you want to start with a list of fuel and cross it off or tear it off as you go? Or like me, use a note on your phone or a drop down list in your spreadsheet to log it (my blog post here has a template if you’d like to use it)?
My guiding principles are:
- Gluten free with no cross contamination risk (because celiac)
- ~250 calories per hour, eating twice per hour to achieve this
- Each fuel (every 30 min) should be less than ~20g of carb, ~10g of fat, and ~5-10g of protein
- I also want ~500mg of sodium each hour through the 2x fuel and when needed, electrolyte pills that have 210mg of sodium each
- Dry food is harder to swallow; mouthfeel (ability to chew and swallow it) is something to factor in.
- I prefer to eat my food on the go while I’m run/walking, so it should be all foods that can go in a snack or sandwich size baggie in my vest. Other options (like chicken broth, soup, and messy food items) can be on my backup list to be consumed at the aid station but unless I have a craving for them, they are secondary options.
- Not a hassle to make/prepare/measure out into individual serving sizes.
Find foods that you like, figure out your guiding principles, and keep revising your list as you find what options work well for you in different situations and based on your running needs!
 )
)



 I went slow the first lap (part of why I was feeling so strong), and I took my time in between laps. I pulled off my socks and shoes. I used hand sanitizer on them to draw some of the water out, then re-lubricated and added Desitin (to continue to help draw water out of my feet and aid in preventing blisters). Then I put on a fresh pair of toe socks and added more lamb’s wool in between key toes that typically are blister-prone. At this stage I had no blisters, and other than wet soggy feet was in good shape! Sitting for 10 minutes for my sock and foot care change chilled me, though, and I was happy to start moving again and warm back up.
I went slow the first lap (part of why I was feeling so strong), and I took my time in between laps. I pulled off my socks and shoes. I used hand sanitizer on them to draw some of the water out, then re-lubricated and added Desitin (to continue to help draw water out of my feet and aid in preventing blisters). Then I put on a fresh pair of toe socks and added more lamb’s wool in between key toes that typically are blister-prone. At this stage I had no blisters, and other than wet soggy feet was in good shape! Sitting for 10 minutes for my sock and foot care change chilled me, though, and I was happy to start moving again and warm back up.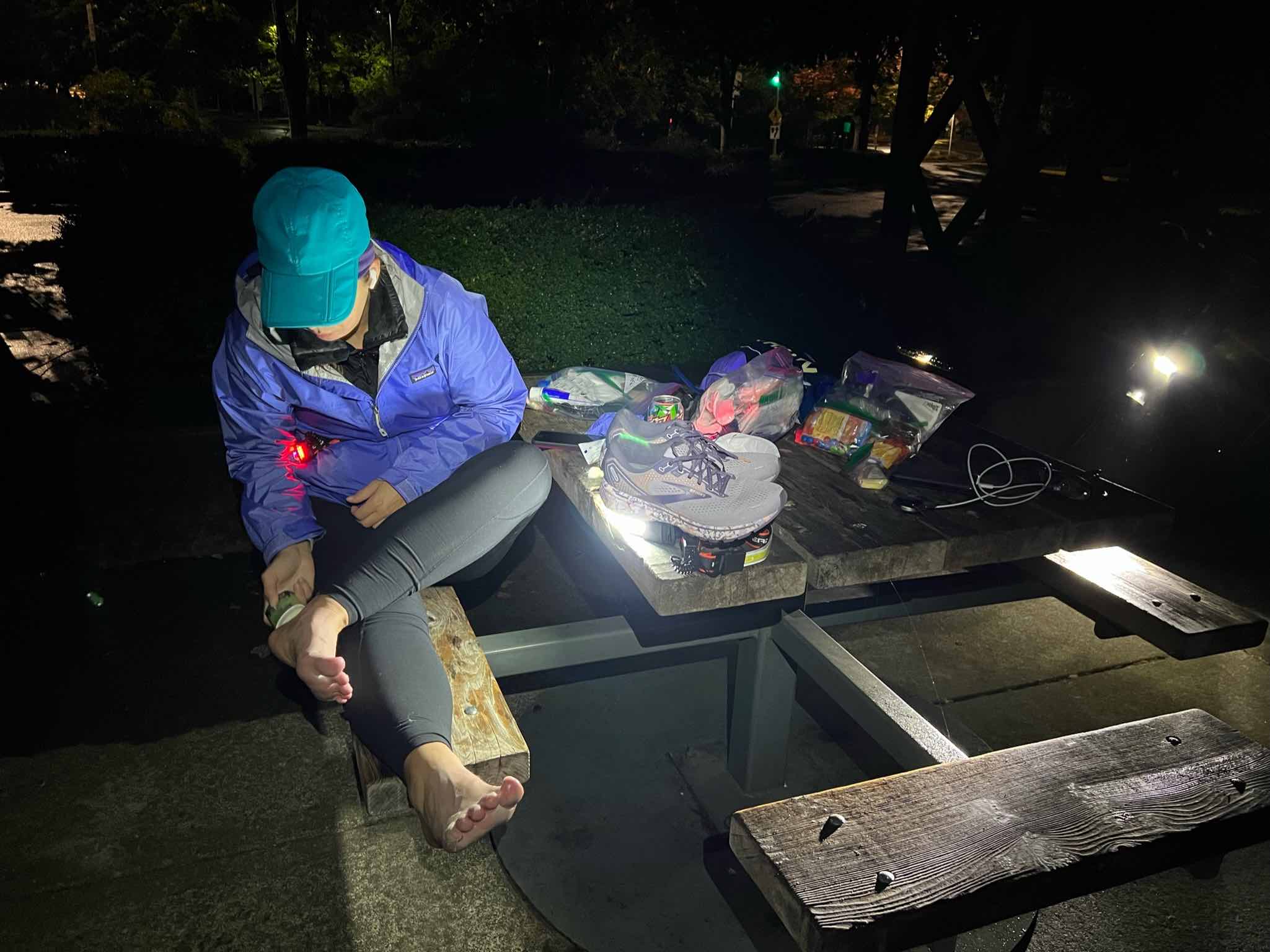

Recent Comments