We’ve learned a lot (from building our own closed loop and watching others do so through OpenAPS) that we think is relevant to anyone who pursues DIY closed looping, regardless of the technology option they choose. This thought process and approach will likely also be relevant to those who switch to a closed loop commercial option in the future, so we wanted to document some of the thought process that may be involved.
Before considering closed looping, people should know:
- A (hybrid or even full) closed loop is not a cure. There will be a learning curve, much like switching to a pump for the first time.
- Even after you get comfortable with a closed loop, there will still sometimes be high or low BGs, because we are still dealing with insulin that peaks in 60-90 minutes; we’ll still get kinked pump sites or pooled insulin; and we’ll still have hormones that drive our BGs up and down very rapidly in ways we can’t predict, but must react to. Closed looping helps a lot, but there’s still a lot that goes into managing diabetes.
Before using a DIY closed loop, people should consider:
- Identifying or creating the method to visualize their data in a way they are comfortable with, both for real-time monitoring of loop activity and retrospective monitoring. This is a key component of DIY looping.
- Running in “open loop” mode, where the system provides recommendations and you spend days or weeks analyzing and comparing those recommendations to how you would calculate and choose to take action manually.
- Based on watching the “open loop” suggestions, decide your safety limits: you should set max basal and bolus rates, as well as max net IOB limits where relevant. Start conservative, knowing you can change them over time as you watch and validate how a particular DIY loop works with your body and your lifestyle.
Getting started with a DIY closed loop, people should think about the following:
- Understand how it works, so you know how to fix it. Remember, by pursuing a DIY closed loop, you are responsible for it and the operation of it. No one is forcing you to do this; it’s one of many choices you can and will make with regards to how you personally choose to manage your diabetes.
- But even more importantly, you need to understand how it works so you can choose if you need to step in and take manual action. You should understand how it works so you can validate “this is what it should be doing” and “I am getting the output and outcomes that I would expect if I were doing this decision making manually”.
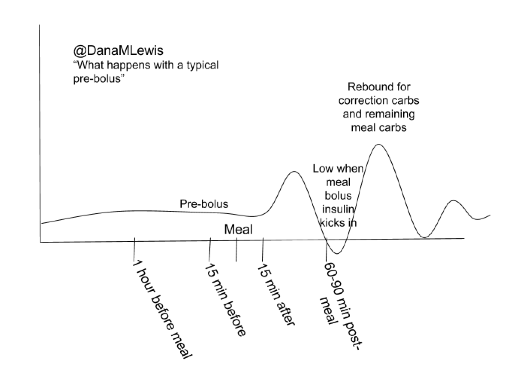
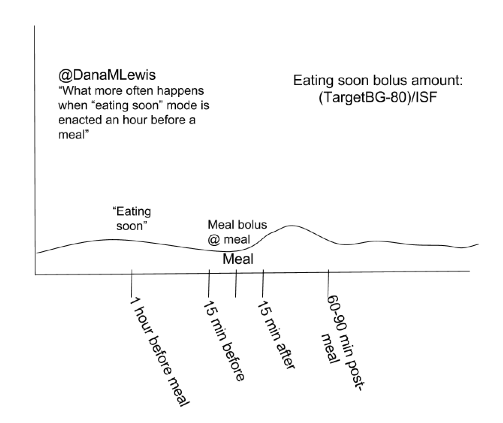
- Often, people will get frustrated by diabetes and take actions that the loop then has to compensate for. Or they’ll get lax on when they meal bolus, or not enter carbs into the system, etc. You will get much better results by putting better data into the system, and also by having a better understanding of insulin timing in your body, especially at meal times. Using techniques like “eating soon mode” will dramatically help anyone, with or without a closed loop, reduce and limit severity of meal spikes. Ditto goes for having good CGM “calibration hygiene” (h/t to Pete for this phrase) and ensuring you have thought about the ramifications of automating insulin dosing based on CGM data, and how you may or may not want to loop if you doubt your CGM data. (Like “eating soon”, ‘soaking’ a CGM sensor may yield you better first day results.)
- Start with higher targets for the loop than you might correct to manually.
- Move first from an “open loop” mode to a “low glucose suspend” type mode first, where max net IOB is 0 and/or max basal is set at or just above your max daily scheduled basal, so it low temps to prevent and limit lows, but does not high temp above bringing net IOB back to 0.
- Gradually increase max net IOB above 0 (and/or increase max basal) every few days after several days without low BGs; similarly, adjust targets down 10 points for every few days gone without experiencing low BGs.
- Test basic algorithms and adjust targets and various max rates before moving on to testing advanced features. (It will be a lot easier to troubleshoot, and learn how a new feature works, if you’re not also adjusting to closed looping in its entirety).
 And if you’re looking to DIY closed loop before a commercial solution is available, you might also be interested in checking out the OpenAPS Reference Design and some FAQs related to OpenAPS.
And if you’re looking to DIY closed loop before a commercial solution is available, you might also be interested in checking out the OpenAPS Reference Design and some FAQs related to OpenAPS.
Recent Comments