 I just went scuba diving in Australia* at the Great Barrier Reef, and I took a flash glucose monitor (Libre) with me under the water.
I just went scuba diving in Australia* at the Great Barrier Reef, and I took a flash glucose monitor (Libre) with me under the water.
WHAT! Yes, really. Scuba diving with a Libre. (Your mileage may vary, of course! The Libre receiver is not waterproof in of itself, and obviously not rated/tested for depth. I did some of that testing for myself. See below 😉 )
—
Historically (and you can read more in this post for more detail on what else I do regarding pump, CGM, and everything else for scuba diving with diabetes and other diabetes devices), I only had a CGM that did not work underwater, and did not work for around an hour after I went diving since it would get waterlogged.
A few months ago when Libre was FDA approved in the US, I paid cash out of pocket (for a receiver + 3 sensors) to try it to see how it did compared to my CGM. For most purposes, a CGM still makes sense for me, because I rely on it for closed looping, and on its low and high glucose alarms. But I know from previous dives and other water activities that my CGM doesn’t work well after a long time in (deep) salt water: I often get false-positive highs for an hour (or more) afterward. So for this trip, I was thinking I would wear a Libre sensor for the dive trip, and just scan when I got out of the water, so I didn’t have to do a fingerstick test after every dive.
In the weeks leading up to our trip, I also saw a picture and heard rumblings of people going scuba diving and taking their Libre receiver under the water. I couldn’t find any details about it, though: What case? What depth? etc. ARGH.
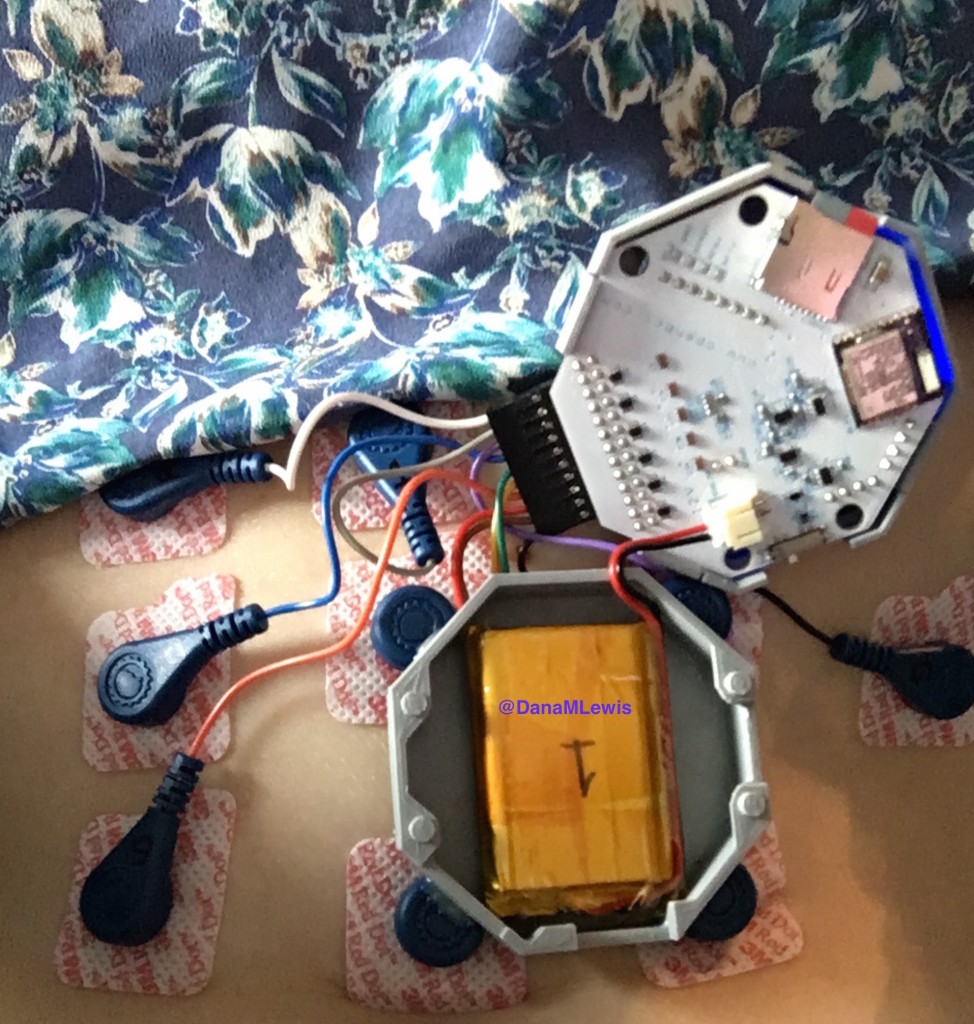
So we decided to pick out a waterproof phone case and just give it a try during our trip. Worst case, we’d just ruin the receiver. Scott found this waterproof phone case/bag (<–Amazon affiliate link) and ordered it, and I packed it for the trip. Probably other similar phone cases would work, too – brand likely doesn’t matter, but you obviously would want a case that’s not going to leak, and should perform a leak test on it before you leave home.
—
We did a “liveaboard” for 3 days and 2 nights (really, ~48 hours on the boat). There’s a transfer boat that takes you out to the “liveaboard”, which is essentially a floating hotel. When you get there, you’re allowed to do a snorkel session before lunch; the first dive briefing is after lunch, and you can then dive during the sessions (max 3 day dives total and 1 night dive) after that during your stay. All this detail to explain that we popped the Libre receiver in the waterproof bag and took it into the water with us when we went snorkeling. And it worked great! So that gave me the courage I needed to take it down during our first dive.
The waterproof case had a strap where you could wear it around your neck, which is what I did. That ended up being annoying occasionally (because the bag would float above you during the die, and sometimes got caught on my snorkel), but it worked. (For future trips I’d probably find a stretchy cord to attach it to my BCD where it was accessible but didn’t have to float or be hung around my neck.)
I wore two wetsuits (I get cold easily!), and even with two layers of wetsuit; the waterproof case; and you know, the water – I was still able to easily press the button on the Libre receiver through the bag, swipe it over my arm, and pick up a BG reading! It was super cool for it to work. The hardest part: finding the Libre sensor under 2 layers of wetsuit on my arm.
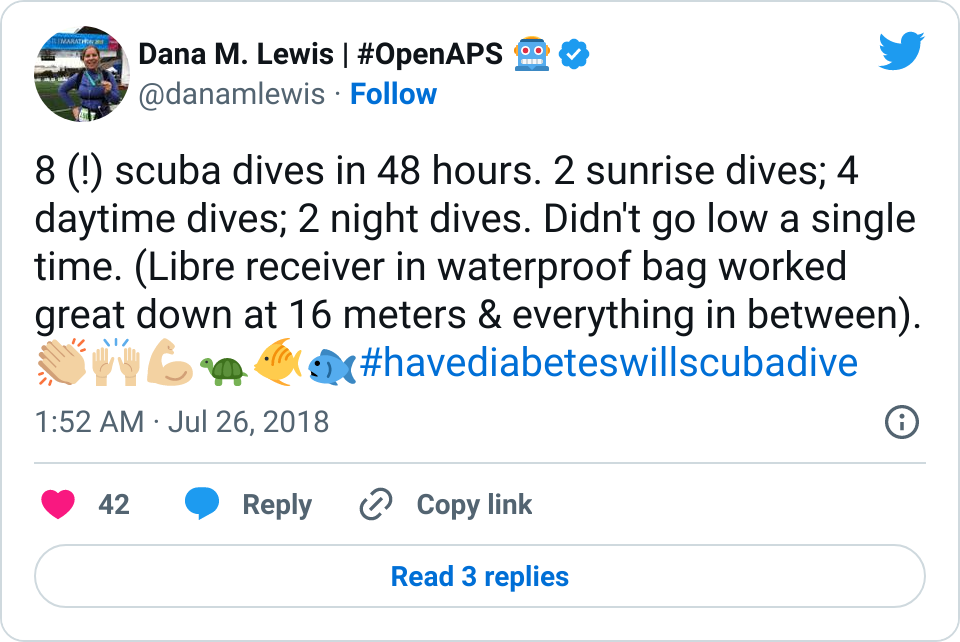
The first few dives were somewhat shallow – 9-12 meters of depth, but over the course of all my dives, I ended up testing it down to 16 meters. I also tested it on 9 total sessions – 1 snorkel, 2 morning sunrise dives, 2 night dives (whoa), and 4 daytime dives. The bag did fine throughout each submersion and never leaked.
I was also expecting the sensor to peel up, so I did four strips of flexifix tape (like I do to my CGM sensor) around the outside edges of the sensor. The tape itself didn’t end up peeling up, and the sensor stayed on just fine! (It probably helped that I wasn’t sunscreening the edges of the tape, since I was pretty much in 2 layers of wetsuit every time I was out in the water and in the sun.) If the sensor ripped out, that would have been a pain as the one I have is the original one approved in the US that requires a 12 hour warmup (ugh) – thankfully, that didn’t happen, and also thankfully, the day we got off the boat we heard that the Libre is now approved in the US for 14 day wear (instead of 10) and now only ONE hour warmup (yay!). That’ll make it nice and easy (if I get the updated sensors) for future dive trips if a sensor rips off.
—
In terms of accuracy and sensor performance:
My first Libre sensor that I had tried at home a few months ago when we got it ran low pretty consistently, and ran REALLY low when my BG was normal. That drove me nuts and I was pretty sure that I wouldn’t want to rely on it the way some people do. So I was planning to not be able to rely on the numbers, and just use it for trends when diving. However, this second sensor (that I did all my scuba diving with) was spot on, even when high and low. I cross checked with finger sticks before and after the first dive, but quickly tailed off fingersticks (other than calibrating my CGM) for the most part, and was able to rely on Libre to double-check my CGM. (As expected, because of the waterlogging, the CGM ran falsely high, sometimes 100 mg/dL off, for about an hour after the dive.)
I left the Libre on even beyond the dive boat part of our trip, and it’s been spot on alongside my CGM (which is also spot on) compared to fingersticks.
—
So to summarize my experience: Libre is great for scuba diving. I tested it down to 16 meters and was happy with how it worked underwater! I loved being able to check mid-dive and see my trends. I never had a low during my 8 dives in 48 hours, and I never worried about going low since I wasn’t diving “blind” to my BGs. I definitely plan to use this for future scuba diving trips, and would also consider using it for any beach/water-based activities. The convenience is worth (for me) paying out of pocket cash for a few sensors to be able to access my BGs easily during these activities.

* One final note: Australia has some of the strictest diving laws in the world regarding your health. If you have type 1 diabetes, you have to have a very particular Australian dive medical form filled out before any company will let you dive. Now, many companies will tell you to just show up in Cairns and use the dive medical centers for a cheap and easy dive medical. HOWEVER: we called three of them in advance. One said “NOPE” out of hand to approving a (perfectly healthy) person with type 1, solely because that person (me) has type 1. The second wasn’t sure and asked us to email a full medical history to give us an opinion. They never responded to the email. The third didn’t answer phone or email. Ugh. So: my advice is, get the form, and go talk **in person** to your physician of choice about this and the necessary information needed to have a physician fill out this form. I stressed a lot about this; but once I handed in the special form along with the standard medical form everyone has to fill out – they didn’t say a word to me, ask me about diabetes, or prevent me from diving. So my advice is to go prepared with your form!















Recent Comments