TLDR: I have newly diagnosed Graves’ Disease, I have associated eye stuff (called “Graves’ orbitopathy” or “Graves’ ophthalmopathy” or “thyroid eye disease”), subclinical hyperthyroidism, and a new learning curve. Below is what I’ve learned so far and what I’m still exploring.
As a person with type 1 diabetes (T1D) – which is an autoimmune disease – I am screened yearly for various high-risk related conditions. For example, celiac disease and thyroid issues, because those are fairly common in people with type 1 diabetes. I already have celiac disease (developed ~6 years after I developed T1D), but we have continued to screen every year in my annual blood work for thyroid markers, usually by screening T4 and TSH. Occasionally, T3 and/or TPO antibodies are also screened.
I remember vividly the chortle that my prior endocrinologist made after we diagnosed my celiac disease in college, probably in response to my comment about being frustrated of having “another” thing to deal with in addition to T1D. He chortled and said something like “once you have one (autoimmune thing), you’re likely to have two. Once you have two, you’ll be likely to have three.”
I didn’t like it at the time, and I don’t like it now. However, he’s not wrong. When your immune system has a little extra kick in it and you develop one autoimmune disease, the rates of having another autoimmune thing are increased. Thus, the typical yearly screening in T1D for celiac & thyroid.
I went 6 years between T1D and celiac, then almost 12-13 years to discover I now have exocrine pancreatic insufficiency (EPI). That’s not necessarily an autoimmune thing but may be a side effect of long-term T1D. Regardless, I was still thankful for the long period of time between T1D and celiac, then T1D+celiac and EPI. I was assuming that something else was coming eventually, but that I’d likely have a few years before the shoe dropped.
Nope.
I wasn’t terribly surprised when I scheduled my annual endocrinology appointment and did my annual blood work to find that one of my thyroid values was off. Specifically, my TSH (thyroid stimulating hormone) was low / below normal range. However, my T4 was smack dab in the middle of normal range. I got my blood work back Tuesday and waited for my virtual appointment on Friday to discuss in detail with my endocrinologist.
Since I’m me, I was curious about the interplay between normal thyroid levels (T4, and I suspected my T3 was likely still in range) but a low TSH value. What did that mean? General consensus seems to define this as “subclinical hyperthyroidism”. It’s not always treated, unless you are older (>65), have osteoporosis or heart disease, or TSH levels are <0.1.
I’m <65, don’t (as far as I know) have osteoporosis or heart disease, and my TSH levels are between 0.1 and 0.4, which is the low end of the normal range. So general treatment guidelines (see this example from the AAFP) suggest treatment isn’t necessarily warranted.
However…there’s more information that factors into the decision making. First, I had my last annual eye exam in October. All was well. Yet in November, I developed really gritty, dry eyes and went in for an appointment. I was diagnosed with dry eyes (gee, thanks!) and recommended to use gel drops at night before bed and regular eye drops during the day as needed. I did end up needing eye drops several times every day.
Then at the end of December or early January, we realized I had exocrine pancreatic insufficiency (EPI). I had been wondering if my dry eyes was related to the lack of digestion and absorption of nutrients, which also influences how my body uses the water content from food. It did seem to get a little better in the following months, because while I still needed the eye gel at night, I eventually moved to several days a week where I didn’t seem to need the eye drops during the day – yay!
However, in February and early March, I started to physically notice a shift in my resting overnight heart rate (HR). My Pebble 2+ HR watch and my Oura ring, both of which measure HR and heart rate variability (HRV), confirmed that both metrics were getting worse. I had a slowly increasing overnight HR and associated decrease in HRV. I am used to fluctuations, because the intensity of my ultrarunning can also influence HR the next day as a signal for whether my body has recovered yet or not. But instead of a day or two of increased numbers, I had an increasing trend line over several weeks, and it started to physically become bothersome. I actually raised the idea of getting my thyroid blood work done early this year, and was about to request the lab work, when after ~6 weeks or so the trend seemed to reverse and things (HR-wise) went back to “normal” for me.
Then I broke my toe in July and the same thing happened, but I chalked it up to sleep disruption from the pain and recovering from the fracture. My HR was continuing to rise even as the pain subsided and my toe was clearly healing. And looking back at my HR data, I can see it actually started to rise at the beginning of July, about two weeks before I broke my toe, so it’s not solely influenced by my broken toe.
As a result of these HR increases (that are noticeable and bothersome because I’m also not sleeping well at night and I physically feel the higher HR during the day), and the ongoing dry/gritty eyes, I suspected that the cause of my “subclinical hyperthyroidism” was Graves’ disease.
I’ve seen estimates that ~30% of people with Graves’ disease have what is called “Graves’ orbitopathy” (and other estimates suggest 20-50%, like this one), so the combination of my ongoing eye symptoms and the low TSH suggested that further lab work assessing various thyroid antibody levels would be able to confirm whether Graves’ disease was the likely source of the subclinical hyperthyroidism.
Therefore, I wasn’t surprised during my virtual visit that my endocrinologist ordered additional labs (repeat of T4 and TSH; adding in T3, TPO antibodies, and TSI (Thyroid Stimulating Immunoglobulin), Thyrotropin Receptor Ab, and Thyroglobulin Ab). Treatment plan, if any, would be based on these results.
I managed to get in that (Friday) afternoon for the repeat lab work, and my results started trickling in by the time I woke up Saturday morning. First, T3, T4, TPO, and TSH came back. T4 was still normal; as I expected, T3 was also normal. TPO antibodies were high, as expected, TSH was still low, as I expected. Saturday night, Thyroglobulin Ab came back high, as expected. Monday, TSI came back high, as expected. Tuesday, my last test result of Thyrotropin Receptor Ab came back, also high as expected.
The summary was: all antibodies high; TSH low; T3/T4 normal.
My endocrinologist messages me Tuesday afternoon confirming mild Graves’ disease with subclinical hyperthyroidism.
The challenge is that I have normal T3/T4 levels. If those were high, we’d treat based on those levels and use those levels coming back into normal range and any change in antibody levels to assess that things were going well.
But the guidelines for subclinical hyperthyroidism don’t really indicate treatment (except on an individual level based on age, other conditions, or undetectable TSH <0.1, as I mentioned).
However, from what I’ve read, the “eye stuff” seems to be driven not by thyroid levels but by the presence of the increased thyroid antibodies. Treatment would possibly bring down the thyroid antibody levels, which might help with the eye disease progression. But not a guarantee. So my doctor left it up to me to decide whether to treat it or not.
Given the ongoing presence of active eye disease (I haven’t been able to wear my contacts for two weeks right now due to swelling/pain in the eyes, plus itching and redness), and the bothersome heart rate feeling, I have decided to try antithyroid medication. I’ll be on a relatively low dose of an “antithyroid” drug, again with the goal of trying to reduce my antibody levels.
This is why I ended up deciding to write this blog post after all: I have not been able to find any clear treatment guidelines for subclinical hyperthyroidism and Graves’ disease with active eye symptoms (from Graves’ orbitopathy). The literature does suggest that treatment to reduce thyroid antibodies even with in-range T3 and T4, targeting a return to normal TSH levels, may be helpful in reducing Graves’ orbitopathy symptoms. This isn’t well known/established enough to have been documented in treatment guidelines, but does seem to occur in many people who are treated.
So hopefully, anyone else with low TSH and high antibodies suggesting Graves’ disease but normal T3 and T4 levels that suggests subclinical hyperthyroidism and also has other symptoms (whether that’s heart rate or other common hyperthyroid symptoms like increased sweating, shaking, heart palpitations, heat intolerance, sleep disturbances) that are bothersome, now have an example of what I chose, given my situation as described above.
I also thought sharing my question list at different stages for my endocrinologist would be helpful. After I saw that I had low TSH and in range T4, and suspected this meant I had subclinical hyperthyroidism from Graves’ disease, given my eye symptoms, the questions I asked my endocrinologist were:
- What additional lab work did we need to confirm subclinical hyperthyroidism and Graves’ disease as the cause? What additional information or lab work would give us a treatment plan?As expected, he repeated TSH and T4, added T3 and TPO and the other antibody tests described above: TGAb, TRab, TSI. This would confirm subclinical hyperthyroidism and Graves’ as the likely source.
- Do I need treatment, since the guidelines generally don’t suggest treatment with normal T3/T4 and TSH between .1 and .4?Initially he suggested treatment would be an option, and after the repeat and expanded lab work, left it up to my decision. Given my symptoms that are actively bothering me, I’m choosing to try low-dose antithyroid medication.
- For hyperthyroidism treatment, beta blockers seem to be part of treatment guidelines for managing symptoms in the short-term, since it takes ~6 weeks for antithyroid medication to show up in lab results. Were beta blockers warranted in my case?My endo typically doesn’t like to prescribe beta blockers unless there are extreme symptoms. He gave an example of someone with a T4 (I think) around 10 and extreme visible shaking. He left it up to me, but his opinion was the side effects, such as lethargy, would outweigh the benefits for mild symptoms, so it is better to treat the root cause. I agreed and did not ask for a beta blocker prescription.
- I also asked if a DEXA scan was warranted to check my bone density.I haven’t had one in over a decade, and celiac and EPI and now Graves’ puts me at possible higher risk of bone density issues. And, since the presence of osteoporosis changes the treatment recommendation for subclinical hyperthyroidism, we agreed it was worth doing. I have it scheduled in a few weeks. My last one over a decade ago was normal.
- Finally, I asked about my eye care, now that I have a known eye thing (Graves’ orbitopathy). Do I need to get referred to an ophthalmologist, or can I continue to see my existing optometrist for annual eye care (including diabetes eye exam) and contact fittings?My endocrinologist suggested that my optometrist can continue to manage my eye care, unless something changes significantly. Ophthalmologists, based on his response and my research, seem to handle severe eye disease treatments that aren’t likely warranted for me. I’ll probably need supportive eye care (e.g. gel drops, regular eye drops) for now. However, I’m planning to send a note to my eye doctor and flag that I want to talk about Graves’ eye things and a plan for monitoring severity and progression over time, and check whether she’s comfortable supporting me or if she prefers to refer me to someone else.
After my repeat labs came back, my endocrinologist messaged me to confirm things and ask if I wanted him to send in the prescription as previously discussed. This exchanged answered the additional questions I had at this time:
- What is the treatment timeline? How soon might I see results?He suggested repeat labs at the 2 month mark. Ideally, we’d see reduced antibody levels and my hope is that my eye symptoms will have also improved and/or I won’t have any additional weeks without being able to wear contacts.
Given I have a clear impact to my heart rate, I’m hypothesizing that I might see changes to the trend in my heart rate data sooner than 6 weeks – 2 months, so that’ll be interesting to track!
- Side effects?Common side effects with antithyroid drugs are rash/allergic type response, headache, or agranulocytosis. He told me to discontinue and contact the office if I had any of those symptoms.
He didn’t go into detail, but I’ve read about agranulocytosis and it seems like if you have a fever and strong sore throat, you need to discontinue and probably will have blood work ordered to make sure your white blood cell counts are ok. Don’t google too much on this one as it sounds scary, but it’s also rare – less than 2% of people seem to have this.
- The only question he didn’t answer was whether it makes a difference in efficacy to take the antithyroid drugs at night or in the morning.Probably, the answer is it doesn’t matter, and whatever time you can take it consistently is best. However, I want to optimize and get the best results from taking this, so I’m bummed that there doesn’t seem to be any evidence (let me know if you’ve found anything in medical literature) suggesting how to optimize timing of it.
So that’s where I am today.
I now have type 1 diabetes, celiac disease, exocrine pancreatic insufficiency, and Graves’ disease (contributing to subclinical hyperthyroidism). It’s possible that we can fix the subclinical hyperthyroidism, and that I won’t need to be on antithyroid medication long-term. However, the data for those of us with Graves’ orbitopathy isn’t super optimistic compared to those without Graves’ eye disease; so I am managing my expectations that managing my thyroid antibody and hormone levels will be an ongoing thing that I get to do along with managing insulin and blood sugars and managing pancreatic enzymes. We’ll see!
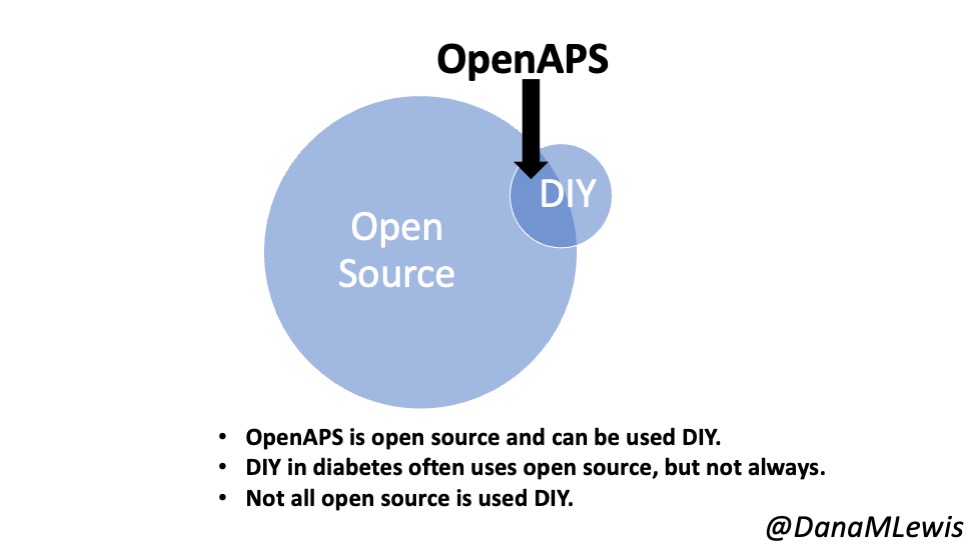
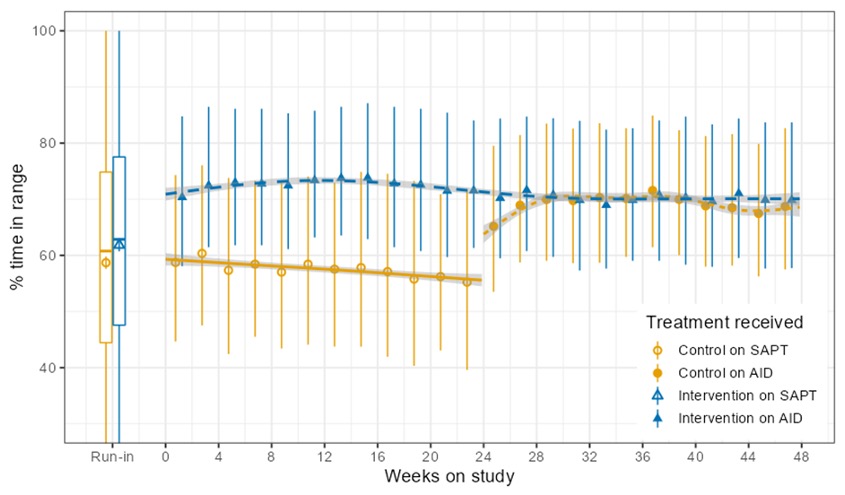
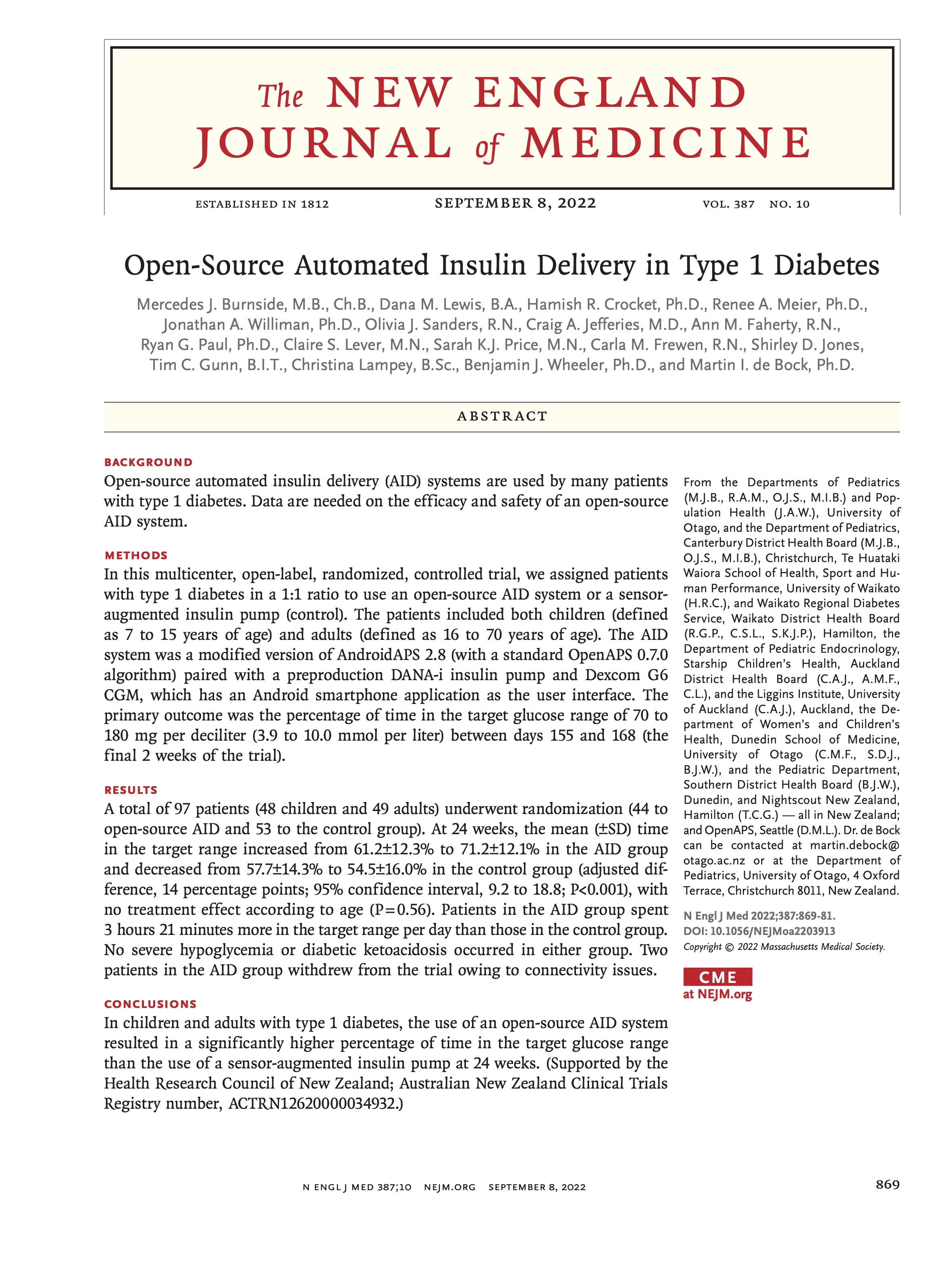 I’m thrilled to share that the results of the first RCT on open source automated insulin delivery (AID) is now published in a peer-reviewed medical journal (New England Journal of Medicine, known as NEJM). You can find it at NEJM
I’m thrilled to share that the results of the first RCT on open source automated insulin delivery (AID) is now published in a peer-reviewed medical journal (New England Journal of Medicine, known as NEJM). You can find it at NEJM 


Recent Comments