(Things I didn’t realize were involved in open-sourcing a DIY artificial pancreas: writing “yes you can” style self-help blog posts to encourage people to take the first step to TRY and use the open source code and instructions that are freely available….for those who are willing to try.)
—
You are the only thing holding yourself back from trying. Maybe it’s trying to DIY closed loop at all. Maybe it’s trying to make a change to your existing rig that was set up a long time ago. Maybe it’s doing something your spouse/partner/parent has previously done for you. Maybe it’s trying to think about changing the way you deal with diabetes at all.
Trying is hard. Learning is hard. But even harder (I think) is listening to the negative self-talk that says “I can’t do this” and perhaps going without something that could make a big difference in your daily life.
99% of the time, you CAN do the thing. But it primarily starts with being willing to try, and being ok with not being perfect right out of the gate.
—
I blogged last year (wow, almost two years ago actually) about making and doing and how I’ve learned to do so many new things as part of my OpenAPS journey that I never thought possible. I am not a traditional programmer, developer, engineer, or anything like that. Yes, I can code (some)…because I taught myself as I went and continue to teach myself as I go. It’s because I keep trying, and failing, then trying, and succeeding, and trying some more and asking lots of questions along the way.
Here’s what I’ve learned in 3+ years of doing DIY, technical diabetes things that I never thought I’d be able to accomplish:
- You don’t need to know everything.
- You really don’t particularly need to have any technical “ability” or experience.
- You DO need to know that you don’t know it all, even if you already know a thing or two about computers.
- (People who come into this process thinking they know everything tend to struggle even more than people who come in humble and ready to learn.)
- You only need to be willing to TRY, try, and try again.
- It might not always work on the first try of a particular thing…
- …but there’s help from the community to help you learn what you need to know.
- The learning is a big piece of this, because we’re completely changing the way we treat our diabetes when we go from manual interventions to a hybrid closed loop (and we learned some things to help do it safely).
- You can do this – as long as you think you can.
- If you think you can’t, you’re right – but it’s not that you can’t, it’s that you’re not willing to even try.
This list of things gets proved out to me on a weekly basis.
I see many people look at the #OpenAPS docs and think “I can’t do that” (and tell me this) and not even attempt to try.
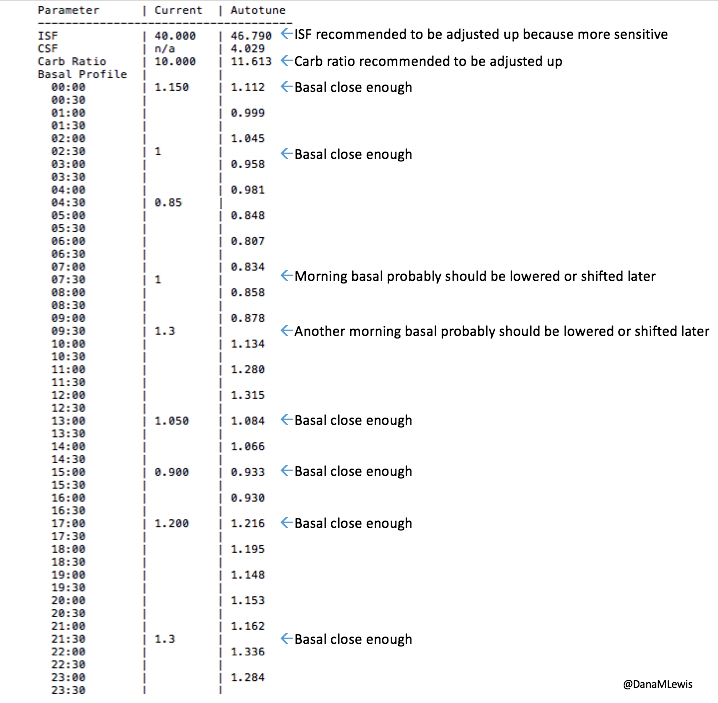
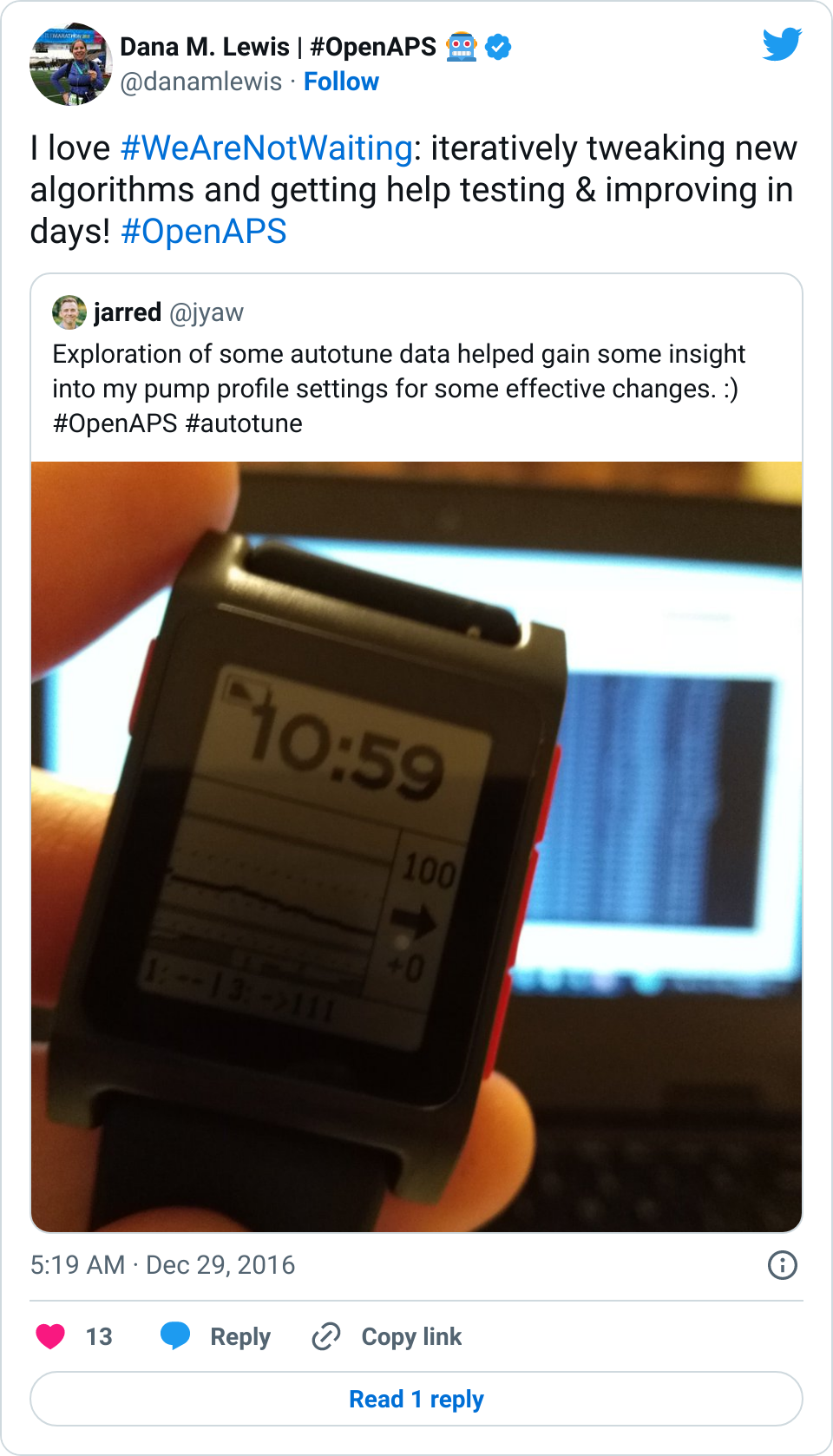
What’s been interesting, though, is how many non-technical people jumped in and gave autotune a try. Even with the same level of no technical ability, several people jumped in, followed the instructions, asked questions, and were able to spin up a Linux virtual machine and run beta-level (brand new, not by any means perfect) code and get output and results. It was amazing, and really proved all those points above. People were deeply interested in getting the computer to help them, and it did. It sometimes took some work, but they were able to accomplish it.
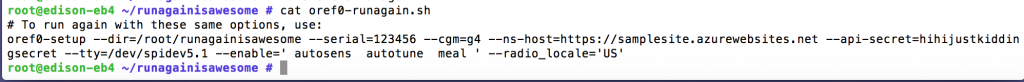
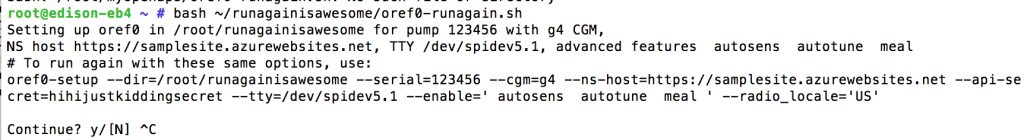
OpenAPS, or anything else involving computers, is the same way. (And OpenAPS is even easier than most anything else that requires coding, in my opinion.) Someone recently estimated that setting up OpenAPS takes only 20 mouse clicks; 29 copy and paste lines of code; 10 entries of passwords or logins; and probably about 15-20 random small entries at prompts (like your NS site address or your email address or wifi addresses). There’s a reference guide, documentation that walks you through exactly what to do, and a supportive community.
You can do it. You can do this. You just have to be willing to try.




Recent Comments