What do you have to do today (related to daily insulin dosing for diabetes) that you’d like to give up if you could? Counting carbs? Bolusing? Or what about outcomes – what if you could give up going low after a meal? Or reduce the amount that you spike?
How many of these 5 things do you think are possible to achieve together?
- No need to bolus
- No need to count carbs
- Medium/high carb meals
- 80%+ time in range
- no hypoglycemia
How many can you manage with your current therapy and tools of choice? How many do you think will be possible with hybrid closed loop systems? Please think about (and maybe even write down) your answers before reading further to get our perspective.
—
With just pump and CGM, it’s possible to get good time in range with proper boluses, counting carbs, and eating relatively low-carb (or getting lucky/spending a lot of time learning how to time your insulin with regular meals). Even with all that, some people still go low/have hypoglycemia. So, let’s call that a 2 (out of 5) that can be achieved simultaneously.
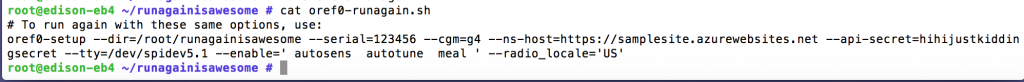
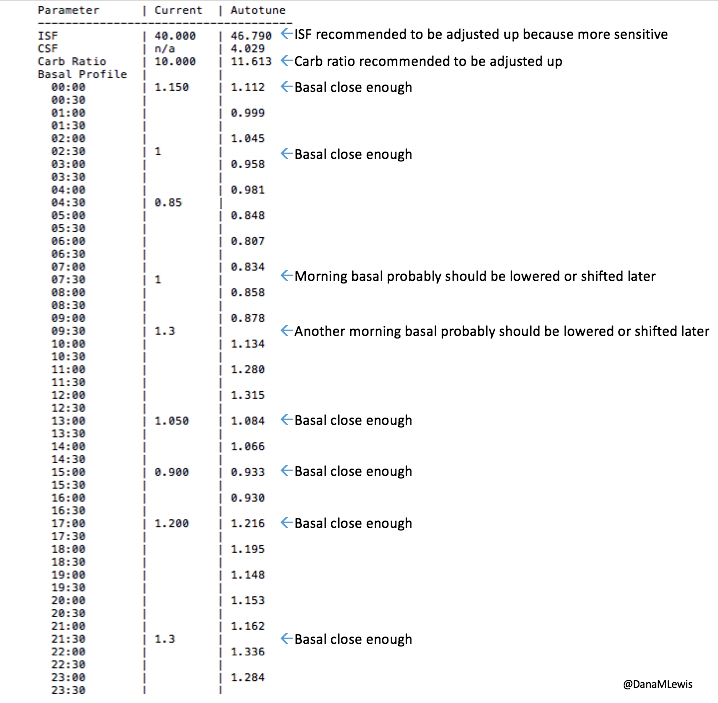
With a first-generation hybrid closed loop system like the original OpenAPS oref0 algorithm, it’s possible to get good time in range overnight, but achieve that for meal times would still require bolusing properly and counting carbs. But with the perfect night-time BGs, it’s possible to achieve no-hypoglycemia and 80% time in range with medium carb meals (and high-carb meals with Eating Soon mode etc.). So, let’s call that a 3 (out of 5).
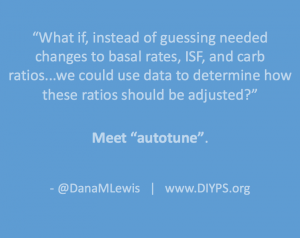
With some of the advanced features we added to OpenAPS with oref0 (like advanced meal assist or “AMA” as we call it), it became a lot easier to achieve a 3 with less bolusing and less need to precisely count carbs. It also deals better with high-carb meals, and gives the user even more flexibility. So, let’s call that a 3.5.
A few months ago, when we began discussing how to further improve daily outcomes, we also began to discuss the idea of how to better deal with unannounced meals. This means when someone eats and boluses, but doesn’t enter carbs. (Or in some cases: eats, doesn’t enter carbs, and doesn’t even bolus). How do we design to better help in that safety, all while sticking to our safety principles and dosing safely?
I came up with this idea of “floating carbs” as a way to design a solution for this behavior. Essentially, we’ve learned that if BG spikes at a certain rate, it’s often related to carbs. We observed that AMA can appropriately respond to such a rise, while not dosing extra insulin if BG is not rising. Which prompted the question: what if we had a “floating” amount of carbs hanging out there, and it could be decayed and dosed upon with AMA if that rise in BG was detected? That led us to build in support for unannounced meals, or “UAM”. (But you’ll probably see us still talk about “floating carbs” some, too, because that was the original way we were thinking about solving the UAM problem.) This is where the suite of tools that make up oref1 came from. In addition to UAM, we also introduced supermicroboluses, or SMB for short. (For more background info about oref1 and SMB, read here.)
So with OpenAPS oref1 with SMB and floating carbs for UAM, we are finally at the point to achieve a solid 4 out of 5. And not just a single set of 4, but any 4 of the 5 (except we’d prefer you don’t choose hypoglycemia, of course):
- With a low-carb meal, no-hypoglycemia and 80+% time in range is achievable without bolusing or counting carbs (with just an Eating Soon mode that triggers SMB).
- With a regular meal, the user can either bolus for it (triggering floating carb UAM with SMB) or enter a rough carb count / meal announcement (triggering Eating Now SMB) and achieve 80% time in range.
- If the user chooses to eat a regular meal and not bolus or enter a carb count (just an Eating Soon mode), the BG results won’t be as good, but oref1 will still handle it gracefully and bring BG back down without causing any hypoglycemia or extended hyperglycemia.
That is huge progress, of course. And we think that might be about as good as it’s possible to do with current-generation insulin-only pump therapy. To do better, we’d either need an APS that can dose glucagon and be configured for tight targets, or much faster insulin. The dual-hormone systems currently in development are targeting an average BG of 140, or an A1c of 6.5, which likely means >20% of time spent > 160mg/dL. And to achieve that, they do require meal announcements of the small/medium/large variety, similar to what oref1 needs. Fiasp is promising on the faster-insulin front, and might allow us to develop a future version of oref1 that could deal with completely unannounced and un-bolused meals, but it’s probably not fast enough to achieve 80% time in range on a high-carb diet without some sort of meal announcement or boluses.
But 4 out of 5 isn’t bad, especially when you get to pick which 4, and can pick differently for every meal.
Does that make OpenAPS a “real” artificial pancreas? Is it a hybrid closed loop artificial insulin delivery system? Do we care what it’s called? For Scott and me; the answer is no: instead of focusing on what it’s called, let’s focus on how different tools and techniques work, and what we can do to continue to improve them.

Recent Comments