Ask me about the time I got a norovirus over Thanksgiving.
As expected, it was TERRIBLE. Even though the source of the norovirus was cute, the symptoms aren’t. (You can read about the symptoms from the CDC if you’ve never heard of it before.)
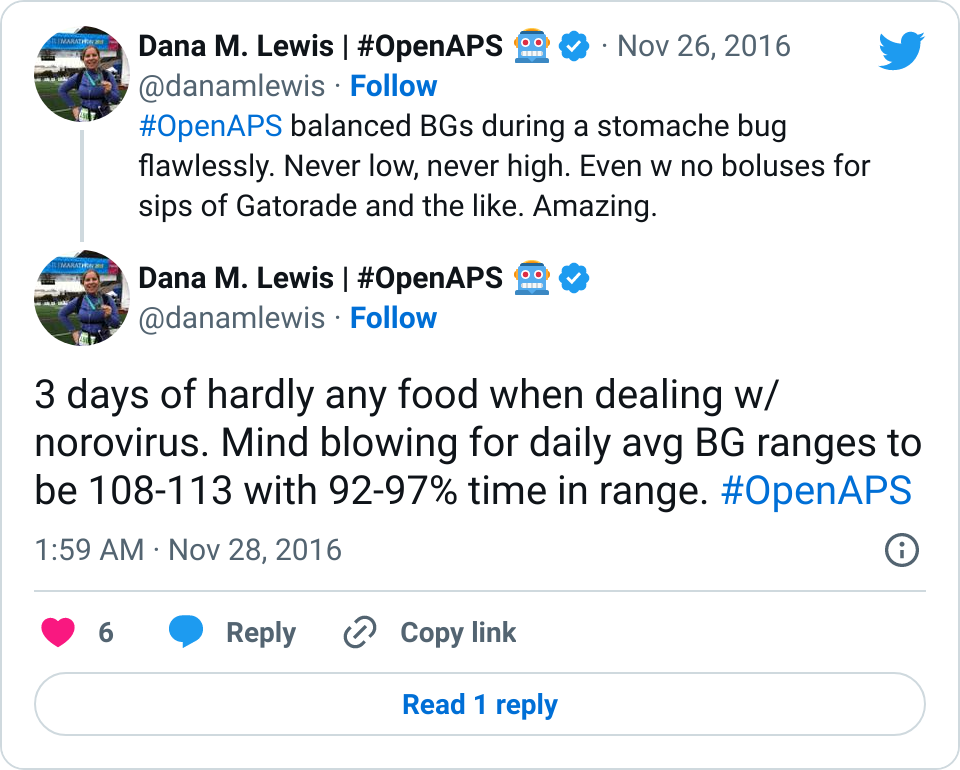
But, unexpectedly, it was only terrible on the norovirus symptoms front. My BGs were astoundingly perfect. So much so that I didn’t think about diabetes for 3 days.
Let me explain.
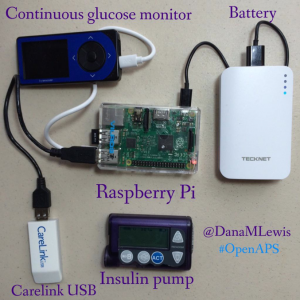
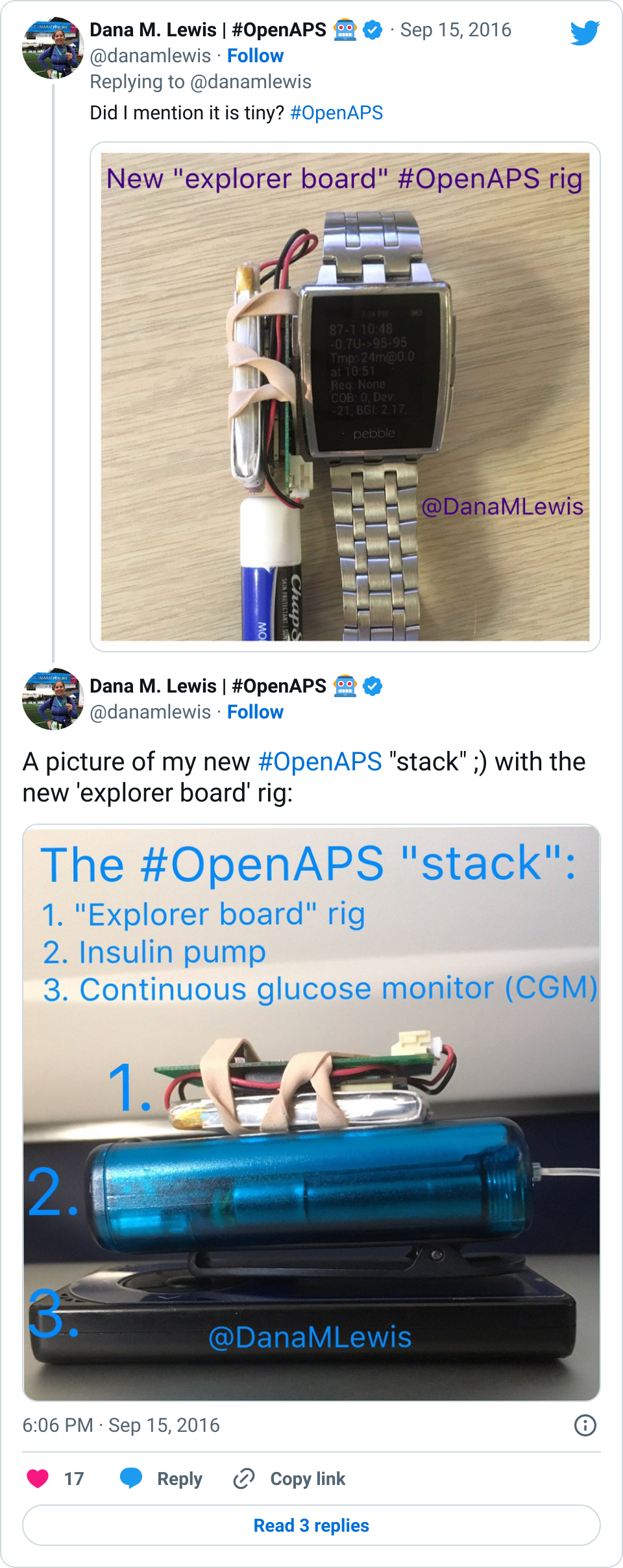
Since I use an OpenAPS DIY closed loop “artificial pancreas”, I have a small computer rig that automatically reads my CGM and pump and automatically adjusts the insulin dosing on my pump.
- When I first started throwing up over the first 8 hours, as is pretty normal for norovirus, I first worried about going low, because obviously my stomach was empty.
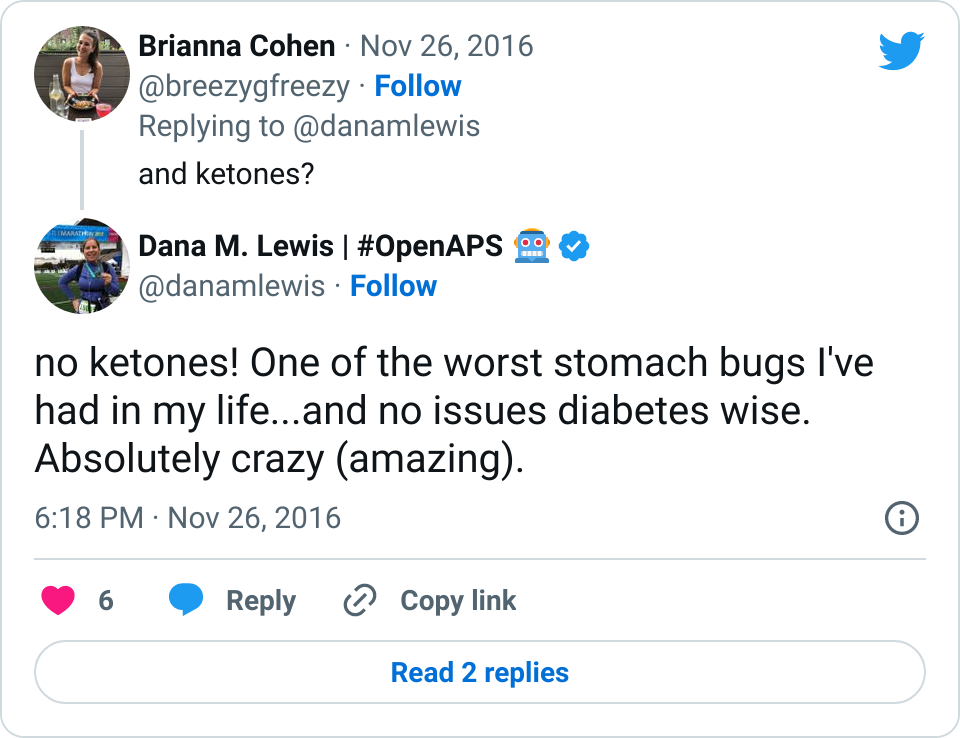
Nope. I never went lower than about 85 mg/dl. Even when I didn’t eat at all for > 24 hours and very little over the course of 5 days.
- After that, I worried about going high as my body was fighting off the virus.
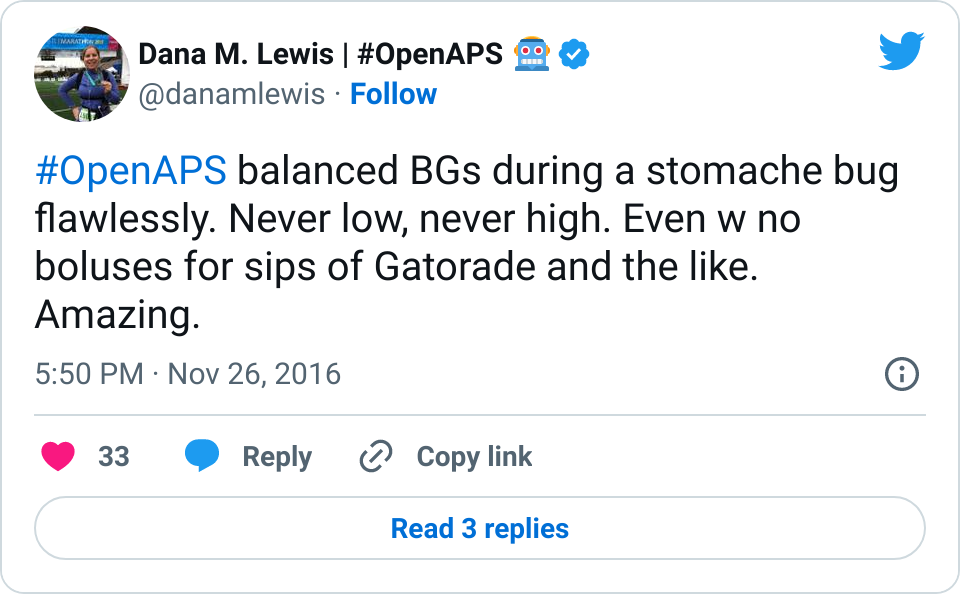
Nope. I never went much higher than a few minutes in the 160s. Even when I sipped Gatorade or gasp, ate two full crackers at the end of day two and didn’t bolus for the carbs.
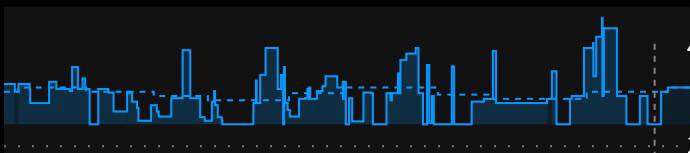
- The closed loop (as designed – read the OpenAPS reference design for more details) observed the rising or dropping BGs and adjusted insulin delivery (using temporary basal rates) up or down as needed. I sometimes would slowly rise to 150s and then slowly head back down to the 100s. I only once started dropping slowly toward the 80s, but leveled off and then slowly rose back up to the 110s.
None of this (\/\/\/\/\) crazy spiking and dropping fast that causes me to overreact.
No fear for having to force myself to drink sugar while in the midst of the worst of the norovirus.
No worries, diabetes-wise, at all. In fact, it didn’t even OCCUR to me to test or think about ketones (I’m actually super sensitive and can usually feel them well before they’ll register otherwise on a blood test) until someone asked on Twitter.
Why this matters
I was talking with my father-in-law (an ER doc) and listening to him explain how anti-nausea medications (like Zofran) has reduced ER visits. And I think closed loop technology will similarly dramatically reduce ER visits for people with diabetes when sick with things like norovirus and flu and that sort of thing. Because instead of the first instance of vomiting causing a serious spiral and roller coaster of BGs, the closed loop can respond to the BG fluctuations in a safe way and prevent human overreaction in either direction.
This isn’t what you hear about when you look at various reports and articles (like hey, OpenAPS mentioned in The Lancet this week!) about this type of technology – it’s either general outcome reports or traditional clinical trial results. But we need to show the full power of these systems, which is what I experienced over the past week.
I’m reassured now for the future that norovirus, flu, or anything else I may get will likely be not as hard to deal with as it was for the first 12 years of living with diabetes when getting sick. That’s more peace of mind (in addition to what I get just being able to safely sleep every night) that I never expected to have, and I’m incredibly thankful for it.
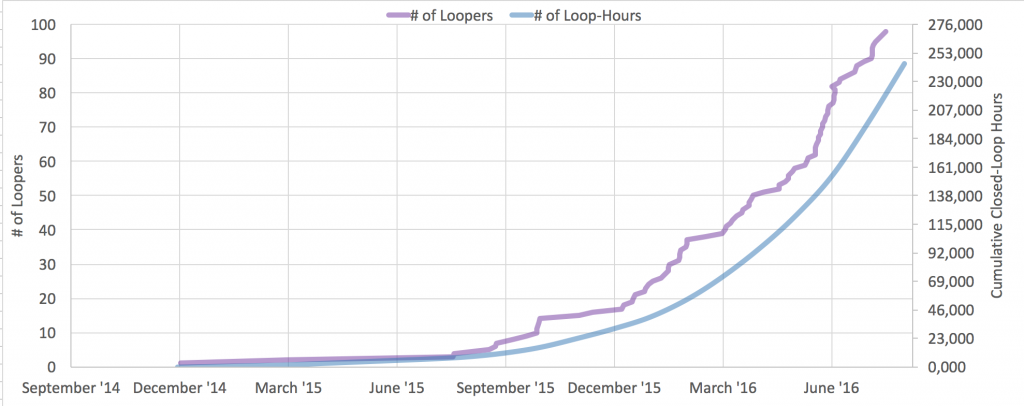
(I’m also thankful for the numerous wonderful people who share their stories about how this technology impacts their lives – check out this wonderful video featuring the Mazaheri family to see what a difference this is making in other people’s lives. I’m so happy that the benefits I see from using DIY technology are available to so many other people, too. At latest count, there are (n=1)*174 other people worldwide using DIY closed loop technology, and we collectively have over half a million real-world hours using closed loop technology.)



 You’re welcome as always to ping me across any channel, but often when there’s a good question, I’m going to want you to re-post in Gitter, anyway, so people can benefit from having the knowledge (including any answers from the community) archived for the next person who has the same or similar question.
You’re welcome as always to ping me across any channel, but often when there’s a good question, I’m going to want you to re-post in Gitter, anyway, so people can benefit from having the knowledge (including any answers from the community) archived for the next person who has the same or similar question.
Recent Comments