A humorous side note – the title of this blog, DIYPS, stands for “do-it-yourself pancreas system”, the name I gave my first automated insulin delivery (AID) system, back in 2013. An AID system doesn’t fully replicate all functions of the pancreas, so we evolved from describing it as an artificial pancreas system (APS) to automated insulin delivery (AID). But now that I have exocrine pancreatic insufficiency and am doing quite a bit of DIY around titration of enzymes….the name of this blog feels more appropriate than ever.
After I started writing about exocrine pancreatic insufficiency, I’ve gotten a lot of questions from friends and connections who think they might have EPI. (And they are likely not wrong – there are estimates that as many as 40% of people with type 1 diabetes have lowered elastase levels. Alone, that doesn’t indicate EPI, but if symptomatic and you’ve already ruled out celiac and gastroparesis, it should be (in my opinion) high on the list of things to test for. Ditto for other types of diabetes and anyone with celiac disease.) Some people, though, may have delays in getting doctor’s appointments, and/or clinicians who aren’t (yet) willing to order the elastase or other EPI-related tests without testing for other things first.
This post is for that group of folks, and anyone stumbling across this post who has seen their test results for their fecal elastase testing indicating they have “moderate pancreatic insufficiency” or “severe pancreatic insufficiency” and are wondering what they can do while they wait for their doctor’s appointment.
It’s also for people with EPI who are struggling to afford their pancreatic enzyme replacement therapy (PERT) or are limiting the number or size of meals they eat as a result of the cost of PERT.
A bit of background on why I did the math about OTC enzyme cost and why I had tested them myself
Due to the holidays in December 2021 I had a lag between getting my test results (over Christmas) and then confirming that my doctor would write a prescription for PERT, and then a delay in getting it filled by the pharmacy since they had to order it. One of the things I did during that time was read up a lot about PERT and also look to see if there were any other kinds of enzymes that would be useful to take if my doctor didn’t want to prescribe me PERT. I found out that PERT contains THREE types of enzymes, and together they’re known as pancrelipase. Pancrelipase contains lipase (helps digest fat), protease (helps digest protein), and amylase (helps digest starches and other complex carbohydrates). It’s typically made from ground up pig pancreas, which is one of the reasons that PERT costs so much. Amylase from non-pancreatic sources is not widely available for human consumption, but there are some other ways to make protease and lipase. And it turns out that these standalone enzyme versions, often produced by microbes, are available to buy over the counter.
While waiting for my test to be ordered, I went ahead and ordered a standalone lipase product that is over the counter (OTC). In part, that was because some of the reviews for lipase talked about having EPI and how they were only sensitive to lipase, and so this was a viable and cheaper alternative for them rather than taking PERT with all 3 enzymes, since they didn’t need that. Based on my experience with FODMAPs and trying an enzyme powder to target fructans (which did help me some), it seemed like trying small doses of lipase would help if I did have EPI, and likely wouldn’t hurt even if I did not have EPI.
And it helped. It didn’t reduce all my symptoms, but even minor doses (3000 units of lipase) made a noticeable difference in my symptoms and I got a sense for what meals were more fat and protein-laden than others.
As a result, when my test results came in and I was on the borderline for moderate EPI, I agreed with my HCP that since it likely wouldn’t hurt to take PERT (other than the cost), and it would be obvious if it helped, that I should try PERT.
So having done the tests with OTC (over the counter) lipase was helpful for deciding to take PERT and advocating for my prescription.
And it turns out, wow yes, I do have EPI and do definitely need PERT (more about my first two weeks on PERT here).
And as I wrote here, because I had the OTC lipase sitting around, even after I finally had access to PERT, I eventually titrated my dosing and calculated separate ratios for lipase:fat and protease:protein, so I can decide for every meal or snack whether I need one full PERT (all three enzymes), two PERT, a PERT plus some lipase (and how much), or just a standalone OTC lipase. The cost differs greatly between those options: one PERT might be $9 and a standalone lipase pill around $0.26. You can’t break apart a PERT (e.g. take only half), so adding a few lipase is a cost-effective approach if you don’t need more protease or amylase and the OTC lipase works for you.
Some of the reasons to explore over the counter enzymes with exocrine pancreatic insufficiency or a suspected case of EPI
One interesting thing about one of the main tests (fecal elastase) used to assess EPI is that it is NOT impacted by taking enzymes. Someone who is started on pancreatic enzyme replacement therapy (PERT) can still have an elastase test without stopping taking PERT. So if someone had an inconclusive result or was borderline and started taking PERT, but their doctor wanted to re-test again, the use of PERT would not affect the test. The same goes for other types of enzymes.
I’ve realized that the following groups of people might want to investigate various OTC enzyme options:
- Someone who has been diagnosed with EPI, but has done careful testing with meals of various sizes (low fat & high protein, high fat & low protein, etc.) to determine that they really only need lipase, may benefit from cheaper lipase-only OTC options.
- Someone who has a test result for EPI but doesn’t yet have an appointment with their doctor or a prescription for PERT could start taking some OTC enzymes for quicker symptom relief, even if they ultimately want to use PERT for all their enzyme needs once they get their prescription filled.
- Someone diagnosed with EPI who cannot afford the ideal dose of PERT that they need for their meals and snacks, may want to calculate the out of pocket costs for OTC lipase (not covered by insurance) vs the cost of PERT with or without insurance.
- Someone who can’t get tested for EPI, but suspects they have EPI, might want to also explore OTC lipase and/or OTC multiple enzyme products.
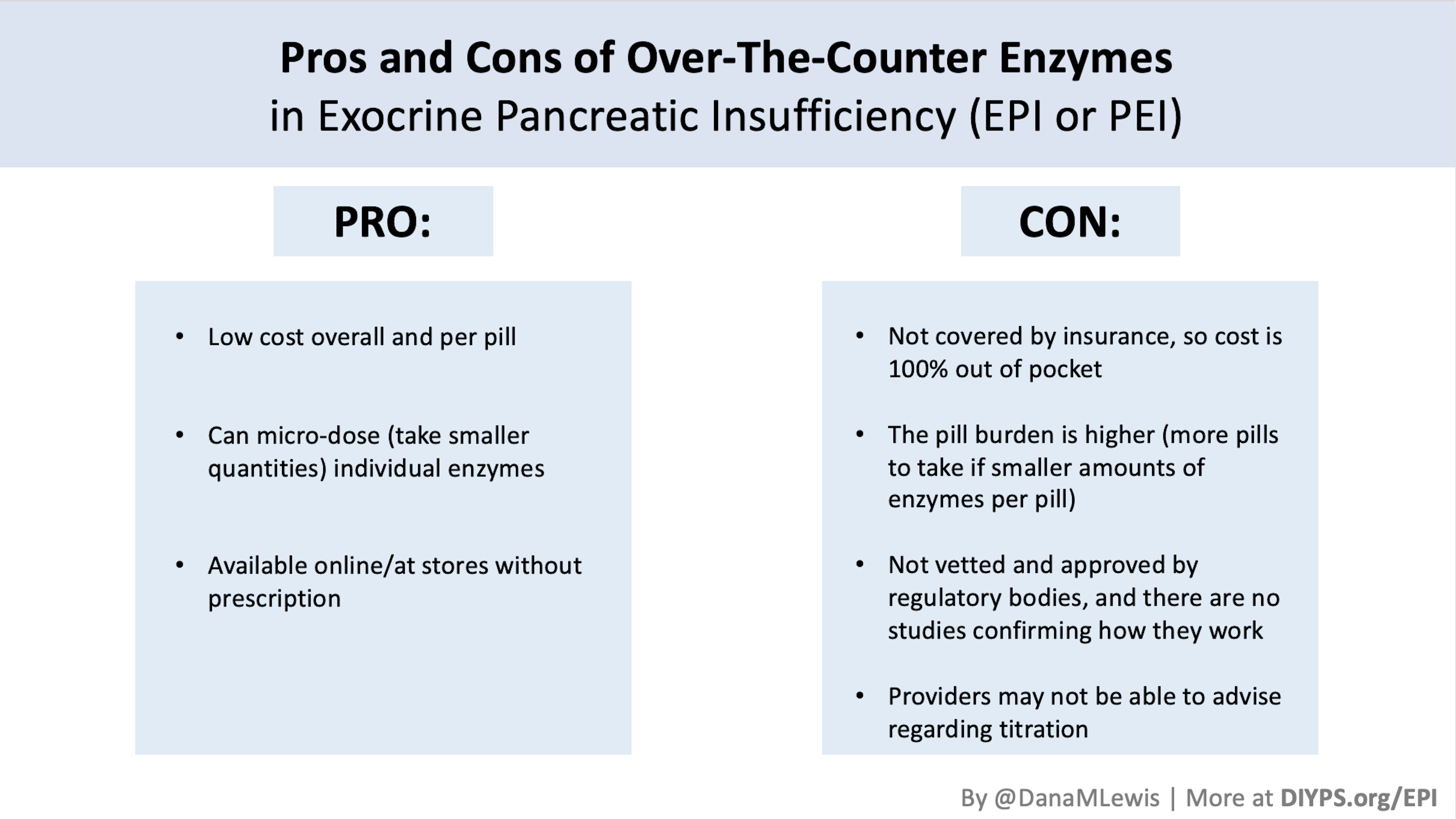
However, not everyone with EPI will want OTC enzymes. Some people may have great insurance coverage, so their PERT costs them less than $9 a pill. OTC enzymes are not covered by insurance, but I’d still do the math and assess what your standard cost is per pill, because it may surprise you how cheap add-on OTC lipase is vs. your insurance deductible or copay to take additional PERT for larger meals. The other reason some people may not want to take OTC enzymes is the pill burden: OTC doses tend to be smaller, so you usually need to take more pills to cover the same meal as a single, larger PERT.
Picking what enzymes (in general, or specific brands) work for you
I often see a variety of OTC enzyme products recommended in peer groups on social media for EPI. There are no studies that I can find assessing the efficacy of these OTC brands (meaning, how good they are). I would be very cautious when trying different single or multiple enzyme products and keep a careful log of your symptoms from before enzymes as well as symptoms at every meal that you take enzymes, and your bathroom results afterward. This can help you assess OTC enzymes as well as PERT if you get access to it. By having a good log of your symptoms, you can tell if you’re taking enough enzymes (OTC or PERT) or if you’re developing new symptoms (which could be a side effect of whatever brand/type you are taking).
There are multiple brands and sizes of PERT, too, and it’s possible that a filler product or how the PERT is made by one brand doesn’t work well for you. If that’s the case, you can try another brand of PERT.
The same goes for OTC enzymes: it is very possible some types of pills may be made with ingredients that could bother you and cause symptoms themselves. You should definitely be very cautious if you go this route and explore small doses and ensure no side effects (no new symptoms) before increasing any doses.
When I search for lipase, it’s easy to find standalone lipase (here is an example, as an Amazon affiliate link). When I search for protease, it’s more common to find products that are multiple enzymes (e.g. lipase AND protease AND other random things that are “good for digestion”). Personally, I’m very wary of anything OTC that’s described as “digestive enzymes” with additional ingredients and prefer to stick to products that only have the ingredients I’m looking for (lipase, protease, and amylase only).
—
The amount of enzyme also matters
The amount of enzyme you take matters, which is probably the second place that people trip up and make mistakes when trialing over the counter (OTC) enzymes. For example, the starting dose recommended for people with EPI is 40,000-50,000 units of lipase. Some of the most common OTC pills have 4-6,000 units of lipase: that means taking 10 OR MORE PILLS per meal in order to get the starting dose. Could you do that? Absolutely. (10 x $0.26 means that is around $2.60 cost, which may still be cheaper than the prescription pills.) However, the burden of consuming that many pills is pretty high in the long run. But you might be ok with that in the short run. There are other OTC options like this one (which I do use myself) that has around ~17,000 units of lipase. They are more expensive per pill, but you have to take fewer (e.g. 3-4 pills per meal) to match the starting dose.
For a lot more info on dosing, read this post about the starting dose and how most people end up needing MORE enzyme than this amount. Then read this post about how to figure out how much enzymes you may need to adjust to the food you’re eating and end up with an optimal dose. (You can also use PERT Pilot to help you with that).
That’s an advanced step, though, so if you’re just getting started I would focus on getting the minimum starting dose (equivalent to 40-50,000 units of lipase per meal) and see how that goes, then titrate (increase) from there.
—
In diabetes, we often say “your diabetes may vary” (YDMV), indicating that different people can have different experiences.
In EPI, it’s no different – “your digestion may vary” and it’s important to test and record and find what works for you, and to find a balance of reducing or eliminating symptoms with enzymes in a cost-effective way that you can afford.
—
(PS, if you didn’t see them, I have other posts about EPI at DIYPS.org/EPI – including one about PERT Pilot, the first iOS app for Exocrine Pancreatic Insufficiency! It’s an iOS app that allows you to record as many meals as you want, the PERT dosing and outcomes, to help you visualize and review more of your PERT dosing data!)
—
You can also contribute to a research study and help us learn more about EPI/PEI – take this anonymous survey to share your experiences with EPI-related symptoms!
—
Thanks for all the information. It has been very useful. I’ve recently started Creon although it’s not working as well even at high doses – I’m close to the max for my weight which is 10,000 lipase units per kg per day. I am considering supplementing with OTC enzymes. I was wondering if you could share which brands you use. I might give it a go. I’m finding the brands and dosing very overwhelming and I’m not sure where to start. Thanks!
Hi Nikki! If you’re close to max doses already, ask your doctor about trying a different brand of approved enzymes. Some people have challenges with one type but do better on another! (E.g. if you’re on Creon, ask about Zenpep or one of the others). If that doesn’t work, some people need PPI added to their PERT. So I would definitely go down that route and talk about it with your doctor!
Thank you Dana for your very thorough and insightful blog!! As someone newly diagnosed with EPI, I’m enjoying your writing, so thank you for taking the time to write your thoughts and experiences!
Since Creon, Zenpep, et al. pancrelipase meds seems to be at least somewhat enterically coated to reach the small intestine without significant stomach acid breakdown, wouldn’t OTC enzymes (like the Vital Nutrients product you linked … thank you again https://a.co/d/eNvB0wq
https://a.co/d/eNvB0wq
require or be better utilized with a proton pump inhibitor (PPI) like Viokase and any of the non-enterically coated meds? I’m wondering if that introduces new complications (and cost), or if you found the OTC-only formulas effective without a PPI.
The OTC approach is quite interesting, not only for the reasons you outline in your posts to augment PERT, but also because Creon is currently (late July 2023) on manufacturer shortage/back-order. I’m having a hard time filling it, am running out, and haven’t yet gotten my provider to trial another pharma PERT like Zenpep (which doesn’t appear to be on back-order?).
Sending best regards…!
Hi John, thanks for reading and your kind words!
It’s a good question. Based on the literature, one would assume it might be needed with a PPI…however, anecdotally, my n=1 experience with OTCs for small/medium size snacks suggest that it’s not necessary (and many others in the community are taking all OTCs with no use of PPI, including for all their meals). I personally haven’t experimented with full size meals and complete use of OTC only, but if I was running short of prescription PERT, I would certainly do so and feel better approaching the experiment due to knowing my regular OTC use for snacks showed it to be effective. For what it’s worth, my elastase puts me in the mild/moderate category (100-200) and I didn’t have any labs showing malnutrition at the time of diagnosis; I’m not sure if the need for PPI with OTC would be different for people with lower natural enzyme production (reflected via lower elastase levels <100) and/or malnutrition. And of course, some of the response to OTC might be individualized, as is much of our EPI experiences!
I think you're right that for whatever reason, the other prescription brands haven't had backorder problems. I think I've now observed (reported by the community) two bouts of back order of the brand you mention, whereas the other brands don't appear to be having the same supply chain issues, so it might be worth experimenting with other prescription brands for that reason if you can, and also OTC, so you have more options and choices that you know work for you in the future.
Thanks again, Dana! That’s helpful insight, even if n=1 My elastase marker was 79, and between a Genova NutrEval nutrient absorption/utilization test and Diagnostic Solutions GI MAP culture, showed poor absorption and production of fatty acids, possibly due to dysbiosis (e.g. little/no presence of some commensal species like Akkermansia). I may experiment with OTC as an adjunct to or replacement for prescription PERT for snacks (I just like comically saying “snacks” lol
My elastase marker was 79, and between a Genova NutrEval nutrient absorption/utilization test and Diagnostic Solutions GI MAP culture, showed poor absorption and production of fatty acids, possibly due to dysbiosis (e.g. little/no presence of some commensal species like Akkermansia). I may experiment with OTC as an adjunct to or replacement for prescription PERT for snacks (I just like comically saying “snacks” lol 
The issue I’m up against now is having two competing GI specialists – one who’s adamant I have EPI, the other who’s fairly convinced it’s a misdiagnosis
 Back to the drawing board (i.e. more testing…)?!
Back to the drawing board (i.e. more testing…)?!
Thank you so much for your help. One of my neighbors, who also has EPI, guided me to you. I have been taking Creon since November 2022. This summer I started to have horrible symptoms all over again. It was over 2 weeks before I figured out what was wrong. I had thought it was a bad batch of Creon. So I tried several different lot numbers that I had on hand. None worked. I had stored the medication with all my other medicines in a closet that was too hot for the Creon. I killed the enzymes! Then trying to get fresh Creon has been hard because of “manufacturing shortage”. I had been rationing my pills. Still a shortage here in VA. After 2 months of fresh Creon, I am feeling better. Now I keep a thermometer next to my Creon so I don’t make that mistake again.
Oh yikes! That stinks! I’m glad you’re feeling better again!
My doctor recommended otc Perts. I asked about prescriptions and she said that the otc meds were fine. So l don’t really know which is better.
Some people find they can use either. It’s about finding what works for you, which could be based on insurance/cost (some people don’t have insurance coverage for Rx PERT and/or can’t afford copays for Rx); side effect profile (some people have side effects with a particular kind); and what works in terms of efficacy of reducing symptoms (in which pill burden can be higher in OTC because you need more pills to match a higher dose compared to Rx). There may not be a clear “better” or there might be, but it’s very individual to you.