New Systematic Review And Evaluation of Pancreatic Enzyme Replacement Therapy (PERT) Dosing Guidelines and Research for Exocrine Pancreatic Insufficiency (EPI or PEI)
I wrote a new paper evaluating the research behind pancreatic enzyme replacement therapy (aka, PERT) dosing for people with exocrine pancreatic insufficiency (known as EPI or PEI). I decided to do this research and write this paper because in my previous papers on EPI, I saw a lot of inconsistencies in when PERT was studied, how it was studied, and how that research was then used to develop guidelines.
(Big thanks to Julia Blanchette, Jordan Rieke, Claudia Lewis (no relation), Khaleal Almusaylim , and Anuhya Kanchibhatla for collaborating on this research and co-authoring the paper with me!)
You can find an author copy of the paper here, or see it on the journal website here. As a reminder, all my research papers have author copies and you can find them at DIYPS.org/research! I also have several other EPI-related articles.
A note on methods – this is a systematic review, meaning I used keywords to search multiple electronic databases to find articles about exocrine pancreatic insufficiency. I screened articles to make sure they were about EPI in humans and focused on English-language articles. We then reviewed the title and abstract of 2,530 remaining articles (!) that mentioned EPI, and excluded those that were not focused on EPI or a co-condition and unlikely to include guidelines or specific dose information related to EPI. That left 820 articles, which we then screened again looking for the full text and reviewing them for relevancy. I ended up reading 257 papers that we used for the basis of the research described below!
We found 7 key findings from this body of research:
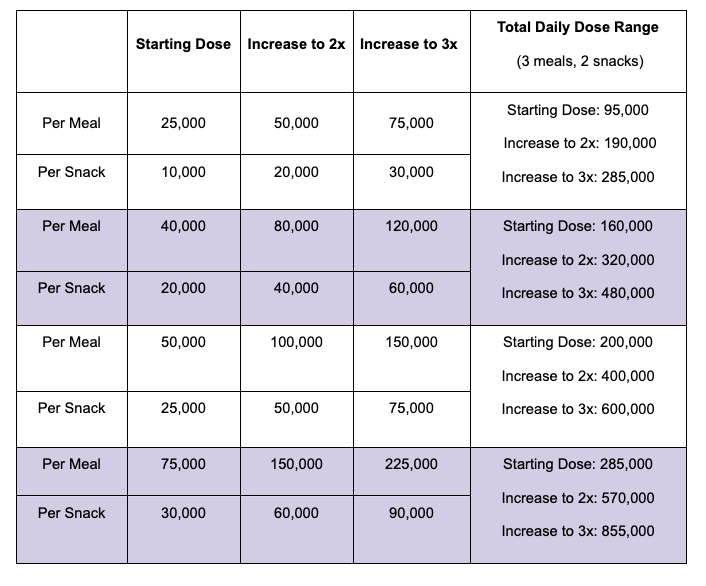
- PERT Titration Protocols Aren’t Very Specific (or useful as typically written)“Most PERT dosing guidelines do not articulate a specific, defined dose range. Instead, PERT is commonly dosed with a general starting dose, such as 50,000 units of lipase per meal and 25,000 units of lipase per snack. If needed, guidelines then recommend increasing (i.e., titrating) the dosage by a factor of two to three (commonly described as increasing by 2x – 3x), and if symptoms persist, adding a proton pump inhibitor (PPI) before exploring other potential diagnoses. As a result, providers are prompted to focus primarily on the starting dose, rather than the full range of recommended doses.”
I ended up crafting a table (Table 2) for the paper that shows how this dosing process can result in much bigger doses – such as 150,000 units of lipase per meal – to contrast how prescriptions are often given at very low doses in comparison and often are not sufficient.This is a similar version of the table that I had developed for a previous blog post talking about the ranges of PERT dosing:
Most guidelines, and the underlying studies, do not do a good job describing what doses people actually took in the studies. This may influence then providers’ understanding of how much PERT is needed.
- People are not taking enough PERTLike I found in my own previous research, there have been numerous studies showing that people are not getting prescribed enough PERT. This is both based on people reporting ongoing symptoms and reduced quality of life, but also studies that show a huge gap between the doses recommended to start with in guidelines and the fact that >90% of the time, providers don’t prescribe anywhere near this dose (and therefore are not prescribing enough PERT).
- Comparing different PERT studies is challengingWhen PERT studies are done, they are typically for safety and efficacy at a specific dose. Very few studies record what dosing people take when they are allowed to take the amount that they need to effectively reduce symptoms.
As a result, we don’t know how much PERT people need (on average) in order to reduce symptoms.
- PERT Dosing Studies and Guidelines Only Focus on Fat (and we need to talk about protein)If you’ve read my previous blog posts about ratios and PERT dosing, you’ll notice I talk about protein dosing. For some people with EPI, protein dosing makes a huge difference in symptom outcomes.
However, PERT is described based on units of lipase (for fat digestion) and primarily studied for fat, which means that doctors often prescribe it and only talk about changing PERT doses for different sized meals based on fat.
This is a huge area of need for future studies to determine what role protein malabsorption plays for people with EPI. I suspect, based on personal experience and talking to others in the EPI community about when they have symptoms, this influences a lot of PERT dosing efficacy in real life.
- PERT Dosing Guidelines Are Very Different Around The World – But Should They Be?There are dozens of PERT dosing guidelines by condition, and in different parts of the world. They don’t always agree!
My hypothesis is that this is not because of a true varying need geographically for PERT dosing (meaning your PERT dosing needs aren’t likely different if you live in South America or Europe), but because of the selection of studies used to determine the guidelines. And because most studies have only looked at basic, minimal doses for safety/efficacy, they haven’t studied how much people need to eliminate symptoms. There’s also no data on what people eat in these studies, so the ‘regional’ differences perceived may be a result of different composition of foods, but we have no evidence for this because the studies are poorly described and/or the studies don’t actually record this.
- PERT Dosing Guidelines Are Different By Co-Condition The majority of the studies on EPI and PERT dosing are in chronic pancreatitis (CP). As I’ve written previously, this is likely a small fraction of the number of people with EPI. But because this body of research on CP and EPI is so big, it has a very loud voice in determining what the guidelines say about PERT dosing. (Cystic fibrosis (CF) is the second-most studied and also plays the second-biggest role in influencing guidelines).
If you want to dig in to the differences between conditions, note that the guidelines are influenced by the volume of studies, and so many conditions (such as diabetes) have very few guidelines and very few studies, so most of the ‘guidance’ on dosing is extrapolated from CF and/or chronic pancreatitis. It’s therefore very possible that people with EPI need more dosing or different dosing than is studied in those co-conditions – but we don’t know more because it hasn’t been studied!
(I have a lot of details in the paper about what has been studied, and you can look at Table 4 for a summary of some of the less-studied conditions or check out the appendix for a narrative description of all of the co-conditions and their bodies of research.)
- PERT Dosing Is Determined By Clinicians And They’re Not Following The GuidelinesMost doctors and clinicians are not following PERT guidelines. This means that many people are prescribed a too-low dose of PERT according to the guidelines. This could be because providers are unaware of the guidelines; or don’t agree with the guidelines; or have not seen evidence showing clear effects of PERT on symptom resolution (in part because this hasn’t been studied!).
More work needs to be done to understand why patients with EPI are under-prescribed and under-dosed when prescribed, and understanding barriers for clinicians may be a key factor to study moving forward.
So, what next?
Here’s what I want to see studied next for EPI, based on the findings in this paper:
- All PERT studies should clearly document the titration protocol in a way that can be understood and reproduced.
- PERT studies should record what dose people take throughout or at the end of the trial.
- PERT should be studied for symptom resolution. (PS – take the anonymous EPI symptom survey if you haven’t already!) This should be done outside of conditions such as chronic pancreatitis, because there is pain associated with CP that is confounding the results of EPI symptoms. And, CP is a tiny fraction of EPI and should not therefore be used to determine whether PERT is effective at resolving EPI-related symptoms.
- We need more awareness of the prevalence of EPI and for clinicians to screen for EPI. When elastase results are low (e.g. less than or equal to 200-ish), providers should initiate a trial of PERT and aid people in increasing their doses to the point that symptoms resolve. We need to study the barriers/factors determining why providers are not screening for EPI and why they are not prescribing PERT.
- We need more tools to help doctors and patients increase PERT dosing to achieve symptom resolution.
- We need studies on the effect of protein in the diet of people with EPI and PERT dosing to improve protein digestion.
If clinicians are reading this, here is your call to action:
- Screen for EPI using a fecal elastase test. This includes anyone presenting with GI symptoms, not just in people that you suspect have chronic pancreatitis. You’re probably missing a not-insignificant number of people coming to you with EPI. For example, a previous systematic review shows EPI is likely much more common in people with diabetes than celiac or gastroparesis!
- If fecal elastase results are around or below 200, prescribe PERT. Yes, even if they’re close to 200 – PERT can help for those with EPI who have symptoms!
This study was published after our systematic review, so I wasn’t able to cite it in the paper, but includes evidence that PERT also can help reduce symptoms when elastase is 200-500. Don’t get too hung up on the elastase result, it’s not very precise but that doesn’t mean you shouldn’t prescribe a trial of PERT. - Prescribe PERT at a minimum of 40,000-50,000 units PER MEAL and tell patients specifically to increase dosing as needed, such as when they’re eating larger meals. Many people need much larger doses (evidence here). Give guidance on how to adjust based on meals. If you want tools, consider things like PERT Pilot or other calculators to aid in matching dosing to food intake. This matches the recent AGA Clinical Practice Update on the Epidemiology, Evaluation, and Management of Exocrine Pancreatic Insufficiency (EPI) by Whitcomb et al which emphasizes that “PERT treats the meal, not the pancreas” meaning that PERT should match food intake.The level of elastase does NOT determine the dosing need, and the size of your prescriptions shouldn’t be influenced by the elastase result.
All EPI needs PERT, and PERT needs should be driven by the individual’s symptoms and the dose it takes to reduce or eliminate their symptoms.
—
Here’s how to cite this paper:
Lewis DM, Rieke, JG, Almusaylim, K, Kanchibhatla, A, Blanchette, JE, Lewis, C. Exocrine Pancreatic Insufficiency Dosing Guidelines For Pancreatic Enzyme Replacement Therapy Vary Widely Across Disease Types. Digestive Diseases and Sciences. 2023. https://doi.org/10.1007/s10620-023-08184-w