In 2002 when I was diagnosed with Type 1 diabetes, I struggled with being handed a vial of insulin and told vaguely to eat X amount of food and take Y amount of insulin. There was no ability to eat more and adjust the dose accordingly. It was frustrating. The only tool I had was a huge (imagine three iPhone 13 or equivalently large smartphones sitting on top of each other) blood glucose meter that took a lot of blood and a long time (a minute or more) to return a single blood glucose data point. The feedback loop wasn’t very useful, even when I tested my blood sugar manually 10-14 times per day.
Thankfully, in the last two decades, diabetes tools have evolved. Meters got smaller, faster, and take less blood. There has also been the devlopment of continuous glucose monitors (CGM) which I can wear and get near real-time readings of glucose data and can see what’s happened in the past. And, paired with an algorithm that also knows about the history of any insulin dosing on my insulin pump, and it can automatically adjust my insulin delivery in real time to predict, prevent, and reduce hypo- and hyperglycemia. (AID is awesome and if you haven’t heard about it, there’s a 4-minute free animated video here that explains it.) Diabetes no longer is quite the headache it was twenty – or even ten – years ago.
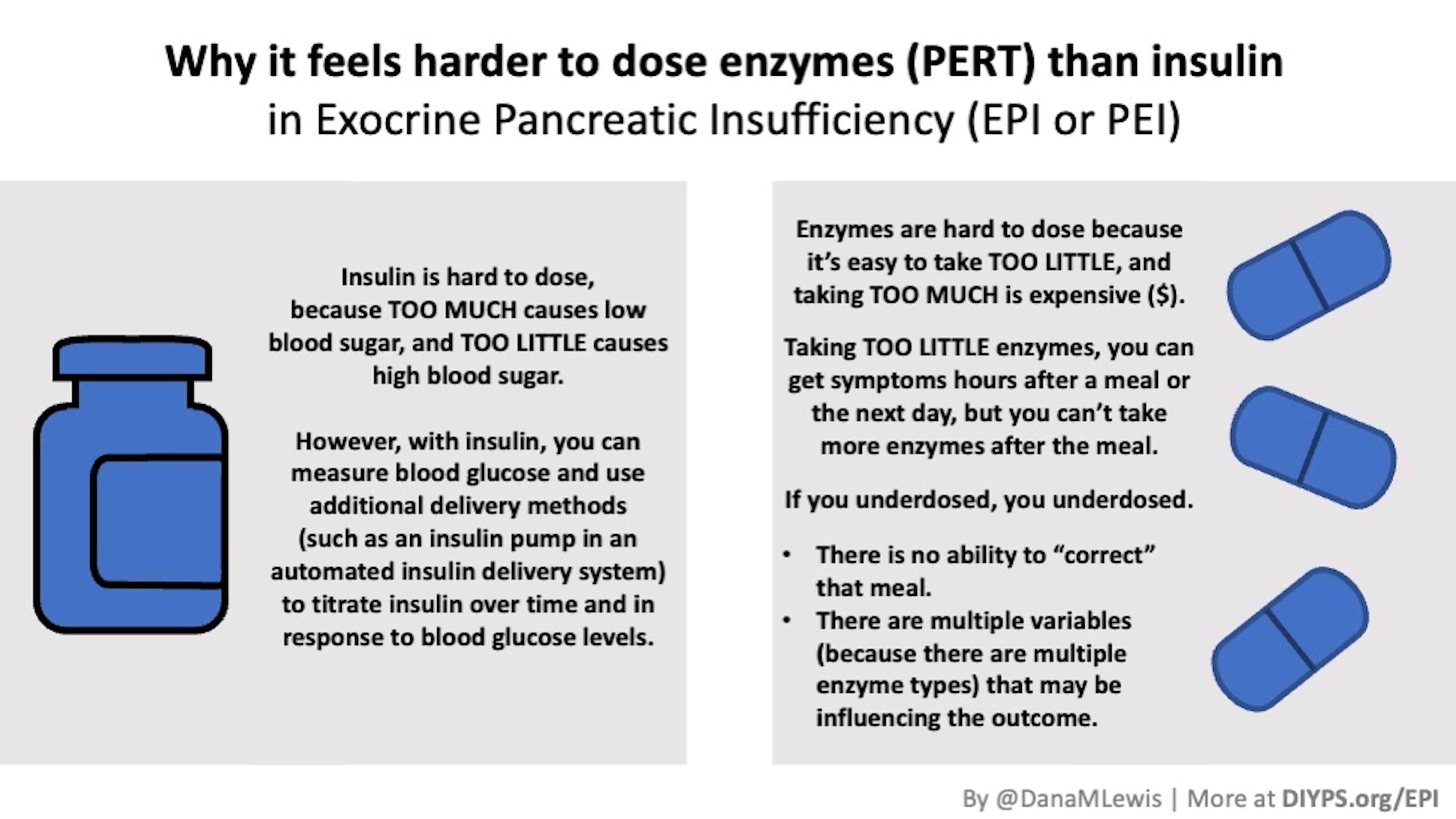
But realizing that I have exocrine pancreatic insufficiency (known as EPI or PEI) and learning how to take pancreatic enzyme replacement therapy (known as PERT) is a similar headache to diabetes in 2002.
With insulin, taking too much can cause hypoglycemia (low blood sugar). Taking too little can cause hyperglycemia (high blood sugar). Yet, with diabetes, you can measure blood glucose and see the response to insulin within a minutes-to-hours time frame. You can also use an insulin pump and an automated insulin delivery system to titrate and adjust insulin in real time.
However, for EPI, you need to take enzymes (that your pancreas doesn’t produce enough of) to help you digest your food. Your pancreas makes three types of enzymes: lipase, to help fat digest; protease, to help protein digest; and amylase, to help starches and carbohydrates digest. These are taken by mouth as a pill that you swallow. Together in one pill, it’s called “pancrelipase”, and it’s for pancreatic enzyme replacement therapy (PERT). (I’m personally bad about using pancrelilpase/PERT interchangeably, because PERT is faster to say and type, but it is possible to use standalone enzymes in PERT).
Because they are pills that you have to swallow when you eat, it’s hard to dose. Taking too little means you may have GI-related symptoms in the hours following the meal and feeling bad until the next day or so. Taking too much is expensive, although unlike insulin it’s rare to take “too much” and cause bad side effects (although possible at super high doses). There’s also the “pill burden”, because swallowing a bunch of pills is annoying and sometimes hard, both physically to swallow and to remember to take them throughout your meal.
You also can’t take more hours later if you forgot to take them or realize you didn’t dose enough for that meal. If you underdosed, you underdosed and just get to experience the symptoms that come with it. Sometimes, it’s not clear why you are having symptoms. Because there are three enzymes being replaced, it’s possible that the dosing was off for any one of the three enzymes. But again, there’s no measurement or feedback loop, or a sign that appears saying “you underdosed protease, take more next time”. The best you can do is try different sized meals over time with different doses of PERT, trying to reverse engineer your lipase:fat and protease:protein and amylase:carb ratios and continuously update them as you have new data.
It’s a lot of work, the feedback loop is slow, getting it “wrong” is painful physically and psychologically, and there are no vacations from it. Everything I eat, now that I have EPI, needs enzymes, and given the fact that I have automated insulin delivery to help manage insulin dosing, I am finding PERT to be a lot harder and more annoying (currently).
—
There’s no happy ending to this post, but this is one of the reasons why I am so interested in partnering with researchers to do research on EPI. There are a LOT of improvements that can be made, ranging from improving titration guidance of PERT to testing the efficacy of different over the counter enzymes to finding new technology that might begin to provide a feedback loop into EPI (either for short-term assessment or longer-term use for those who prefer it). If you’re someone interested in this type of research, please don’t hesitate to reach out (Dana@OpenAPS.org).
—
(PS, if you didn’t see them, I have other posts about EPI at DIYPS.org/EPI – including one about PS – PERT Pilot, the first iOS app for Exocrine Pancreatic Insufficiency! It’s an iOS app that allows you to record as many meals as you want, the PERT dosing and outcomes, to help you visualize and review more of your PERT dosing data! It’s one of the things I decided to build to help address the challenges I know those of us with EPI face every day.)
—
You can also contribute to a research study and help us learn more about EPI/PEI – take this anonymous survey to share your experiences with EPI-related symptoms!
—