As I’ve said many times, last year we set out to create a louder CGM alarm system. By adding “snoozes” so I didn’t drive my co-investigator crazy, we realized I might as well enter what I was doing, and be precise about it (aided by some quick bolus and quick carb buttons that made data-entry not the chore that it sounds). Thus, we had the data and the brains to realize that this made for some great predictions; much better than what you usually see in diabetes tools because they rely only on your insulin sensitivity factor (ISF) and correction rate, but don’t take into account carbs on board and their impact over time, etc.
(If you’re new to #DIYPS, read about the beginnings of it here. For more on this idea of carbs on board and the carbohydrate absorption rate and how significant it is for people with diabetes, read about that here.)
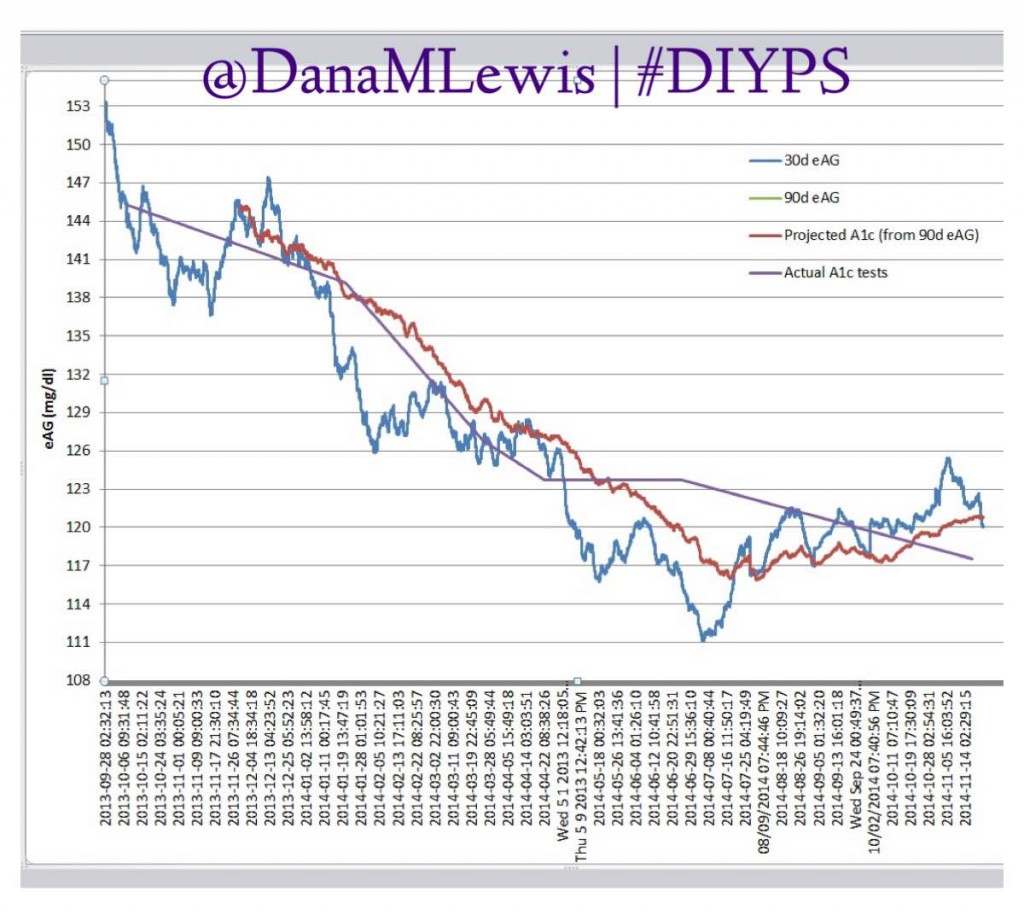
After I had spent 100 days using #DIYPS, Scott and I stopped to look and see what the impact was. For the long version, read this post about the results and the direct comparison to the bionic pancreas trial data that was available then. The short version: #DIYPS reduced my eAG and a1c significantly, reduced lows, reduced highs – aka my time in range was improved from 50% to regularly 80+%.
I have asked myself (and others have asked), are these results sustainable? Are these improved outcomes truly because of #DIYPS? It’s definitely worth noting I never changed what or how I ate. (I ate 120 grams of pizza (for science! ;)) several times to test the system, but I didn’t eat less or any healthier or otherwise change my diet.)
I can’t attribute these outcomes directly to #DIYPS alone, but I do believe they’re highly correlated. It’s hard to separate other contributing factors like the fact that I have more boluses per day using #DIYPS (which other studies have shown decreases a1c); or the fact that I spend less time high/low because with #DIYPS I actually can wake up at night and take action before I’m high or low.
So, it’d be hard to study specific factors and say “it’s all #DIYPS”. But, I’m pretty sure it’s mostly #DIYPS. Regardless, here’s the updated data about the sustainability of the results I’ve seen with #DIYPS over the past year:
Why this is significant
#DIYPS is currently n=1 (meaning one person is the study’s subject). But what is significant is that I have year’s worth of data and actual lab-tested a1cs that shows the outcome of this type of artificial pancreas work. And it (to date, but coming soon / OMG this week!) hasn’t even been closed loop – I’m still the “human in the loop” making decisions and pushing buttons on my pump.Compared to the bionic pancreas and other artificial pancreas study trials where they have a few days and a few more (usually n=20 or so) subjects; they can look at the decrease in lows and highs and improved eAG…but they can only project what the a1c improvement is going to be.We’ve shown the improvements in lab-tested a1cs – see my graph above?
It all adds up
Scott and I are not the only ones working on a closed loop. The community of developers connected to the Nightscout community has nearly two hands full of people who are working independently on device interoperability to close the loop by freeing our data from devices and enabling us to work with our own algorithms regardless of which hardware device we use to support our diabetes management.When all of these n=1 studies add up, it matters. At some point in the near future, after we’ve closed the loop with #DIYPS (ah! this week! :)) and others have as well, we may have more n=1 hours on closed loop artificial pancreas systems than the (traditional) “researchers”. Scott and I are hoping that we can not only show the world how open source innovation and new regulatory paradigms can deliver safe and effective results for people living with T1D faster than traditional medical device development and traditional regulation; but that we can also change how all successful medical device companies approach interoperability, and how traditional medical researchers do research – possibly in partnership with patient researchers like us.
It’s been fascinating to watch the journey you guys have been on. Thank you both for sharing so openly with us.
I developed an insulin bolus calculator using SMBG data, published in Diabetes Care in 1986, . I have developed numerous methods for display of glucose data (e.g., AGP or Ambulatory Glucose Profile, Diabetes Care, 1987; 7 papers in 2009 in JODSAT and DTT), and for evaluation of quality of glycemic control (January 2015, Journal of Diabetes Science and Technology). I have developed several methods for evaluation of glycemic variability using CGM.